You know that sinking feeling when you’re reading an interesting, helpful blog post, and you run into some piece of jargon that stops you like a brick wall?
“… trying to change her AUC …”
“… could be due to GLUT4 transcription …”
“… a condition caused by insulinemia …”
Like any health niche, metabolic fitness has its own vernacular, full of medical words and abbreviations that aren’t always explained. We’ve assembled a list of the most common terms and acronyms associated with all things metabolic to make your health journey a little smoother.
A1c (or HbA1c) test: This blood-sugar test measures the percentage of red blood cells with glucose attached to them. Unlike a fasting glucose test, which captures a moment in time, A1c shows your average glucose levels over the past three months (about how long glucose stays attached to hemoglobin). However, it’s still limited in that it doesn’t reflect daily variations—someone with frequent glucose spikes could still show a “normal” A1c, even though that’s less optimal than stable blood sugar. Always discuss results with your health-care provider, but here’s a rough guide to the numbers:
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or above

What should your glucose levels be? Here’s the ultimate guide to healthy blood sugar ranges
Fasting blood sugar levels classify into 3 categories: normal, prediabetes, and diabetes. To be considered “normal,” fasting glucose must be under 100 mg/dl.
Read the ArticleAdipose: The technical name for fat tissue made up of adipocytes (fat cells), adipose tissue has an endocrine function, releasing several hormones, including leptin, which acts on our appetite, and adiponectin, which affects insulin sensitivity. Adipose tissue can be subcutaneous, or just under the skin (think: belly fat), or visceral, which means around our organs. Dysfunctional adipose tissue can play a role in metabolic syndrome.
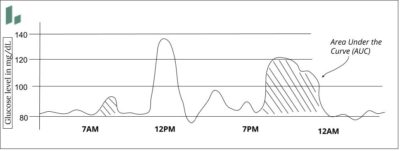
Area Under the Curve (AUC): If you’re plotting glucose values (or any value) as a line on a chart that resembles a rolling hill, the area under the line is the AUC. Talking about AUC is a way of describing both the height of the glucose rise after a meal and the length of time your glucose is elevated. You want lower spikes quick returns to normal, so lower AUC values.
ATP: Short for adenosine triphosphate, this molecule has many functions but in metabolic health it’s essentially the energy currency of our cells. Mitochondria produce ATP through the breakdown of glucose in the presence of oxygen—also known as aerobic or cellular respiration.
Beta cells: Located in the pancreas, these cells create and release the hormone insulin in response to blood glucose. (The same cells also produce related hormones C-peptide and Amylin.) In people with Type 1 diabetes, their immune system attacks beta cells, creating an insulin deficit.
Biomarker: Any measurable medical sign or substance can be a biomarker. Typically used in a diagnostic context, biomarkers for metabolic health include glucose levels, insulin levels, or lipid (cholesterol) levels.
Blood sugar: Technically accurate, if not exactly precise, this is a short-hand for referring to the glucose (a form of sugar) that’s circulating in your blood. All simple carbohydrates are sugars, but when we talk about blood sugar, we mean glucose. The concentration of glucose in your blood is the value measured by a continuous glucose monitor (although it technically measures glucose in the interstitial fluid just under your skin, a close proxy for what’s in your blood).
“While our body needs glucose, too much or too little can cause a range of health problems, from obesity to blindness. That’s why it’s important to make diet and lifestyle choices that help our bodies maintain stable glucose levels.”
Carbohydrate: Carbohydrates are one of the three macronutrients (along with fat and protein) your body uses for energy. A combination of hydrogen, carbon, and oxygen, carbohydrates eventually break down into glucose that powers our cells. Carbs include fiber, starches, and sugars. They can be simple (meaning they have fewer than three sugars and are absorbed and processed quickly, typically leading to a blood sugar spike) or complex (more sugars, longer processing period). Simple carbs include candy and syrup; complex carbs include beans, non-starchy vegetables, and nuts.
CGM: A continuous glucose monitor (CGM) is a small bio-wearable device, meaning it’s something you attach to yourself that measures something going on inside your body. CGMs measure glucose concentration via a tiny probe that sits under your skin and samples the interstitial fluid between the subcutaneous cells, a close proxy for what’s in the blood. CGMs then transmit that data to a smartphone or other device where it’s interpreted and displayed.
Initially developed in the late 1990s for people with diabetes to augment or replace finger-stick glucose tests, CGMs are increasingly used by non-diabetic people to get real-time feedback on their metabolic health.

What is a continuous glucose monitor?
A continuous glucose monitor (CGM) can help you track your blood sugar in real-time. So how does a CGM work, and who should use it?
Read the ArticleEndocrine: The endocrine system encompasses the glands in our bodies that produce and secrete hormones, such as the pituitary, testes, ovaries, and thyroid. It also includes the pancreas, which makes insulin, the primary metabolic hormone. People with diabetes work with endocrinologists, who specialize in these systems.
GLP-1: Short for glucagon-like peptide-1, this hormone has many effects, one of which is to promote insulin secretion in response to glucose. Drugs called GLP-1 agonists can help people with Type 2 diabetes control blood sugar.
Glucose: It’s one of the two primary fuel sources that power our bodies at the cellular level (the other is ketones, derived from fat). Glucose is a simple carbohydrate—a monosaccharide, which means it is a single sugar (sucrose, or table sugar, is a disaccharide composed of glucose and fructose).
Enzymes break down all carbohydrates we eat into glucose, circulating in our blood until insulin either signals cells to absorb it or store it as glycogen for later use.
While our body needs glucose, too much or too little can cause a range of health problems, from obesity to blindness. That’s why it’s important to make diet and lifestyle choices that help our bodies maintain stable glucose levels.

How a CGM can help you find your optimal diet and lower blood sugar
There’s no "ideal" diet for everyone, but a continuous glucose monitor gives you real-time feedback on the foods that work best for your metabolic health.
Read the ArticleGLUT4: This is an acronym for glucose transporter type 4, which is just what this protein does. Signaled by insulin, it’s one of a family of proteins that help muscle and fat tissue absorb glucose from the bloodstream and plays a central role in glucose homeostasis. Defects in GLUT4’s function can play a role in insulin resistance.
Glycation: When glucose molecules circulate in the bloodstream, they can attach to red blood cells in a process called glycation. (Technically, glycation refers to any carbohydrate attaching to a protein.) Glycation is normal, but too much can produce damaging compounds called advanced glycation end products (AGEs) that can cause inflammation and lead to problems from wrinkles to Alzheimer’s disease.
Glycemic Index: The glycemic index (GI) scale is a sort of cheat sheet for how quickly a particular food might raise your blood sugar. High GI foods, such as candy, white bread, or potatoes, have simple carbohydrates the body processes quickly, so they can spike your glucose. Low GI foods include non-starchy vegetables and legumes that take longer to process. (Foods with no carbohydrates such as meat have no GI value).
The glycemic index is useful but imperfect for two primary reasons: 1) We each process foods differently. What spikes you may not spike me. 2) Many other factors, including stress and sleep, affect how our body processes food.
Hyperglycemia: High glucose levels. Fasting hyperglycemia (levels above 130 mg/dL) is a significant indicator of diabetes but can be dangerous even at sub-diabetic values. After-meal (sometimes called postprandial) hyperglycemia describes a blood-sugar spike from eating; for non-diabetics, this should rarely exceed 140 mg/dL.

What should your glucose levels be? Here’s the ultimate guide to healthy blood sugar ranges
Fasting blood sugar levels classify into 3 categories: normal, prediabetes, and diabetes. To be considered “normal,” fasting glucose must be under 100 mg/dl.
Read the ArticleHypoglycemia: Low glucose levels, generally below 70 mg/dL. For non-diabetics, the “crash” after a blood sugar spike can bring on reactive hypoglycemia, which may induce fatigue or a jittery feeling. Drinking alcohol can also induce hypoglycemia, especially if you are fasting or in a ketogenic state.
Inflammation: When your body senses a threat, it sends white blood cells that trigger the production of hormones, such as histamine, that can address the problem. These reactions often produce the symptoms you associate with inflammation, such as swelling or redness. Inflammation also happens inside your body in response to threats like a virus or cellular damage. Chronic inflammation, which can last for months or years, plays a role in many deadly conditions, including cancer and cardiovascular disease.
Inflammation is also a significant factor in metabolic dysfunction. Insulin resistance is what’s called proinflammatory; inflammation is one of the mechanisms through which insulin resistance can do so much damage, from weak tendons to increased risk for COVID.

Inflammation and glucose levels: How high blood sugar can turn a good system bad
Inflammation helps heal your body, but chronic inflammation can cause serious damage. Here’s how a healthy lifestyle—including a low-sugar diet—can help keep it in check.
Read the Article
What causes insulin resistance?
Insulin resistance is a shockingly common condition spurred on by diet and lifestyle. Here are the processes in your body that lead to this dangerous state.
Read the ArticleInsulin: Every cell in our body contains receptors for this hormone. Insulin’s effect depends on the cell. In some cells, like muscle and fat, it stimulates glucose uptake. Most cells in our body don’t need insulin to pull in glucose, but they still need insulin to help them know what to do with nutrients like glucose and fat. Because of its wide-ranging effects across the body, irregular insulin levels can lead to a variety of health conditions.
Insulin Resistance: When cells become “numb” to insulin’s effects—meaning more is needed to accomplish the same task—we say that they are insulin resistant. Several factors can cause IR, but a primary driver is too much insulin, often caused by chronically elevated glucose levels.
Insulin resistance can lead to Type 2 diabetes, but it is also associated with nearly all chronic conditions, including heart disease, infertility, and Alzheimer’s disease. Half of all U.S. adults, and roughly one in three Americans, are known to have it. The good news is that you can reverse it with better diet and lifestyle choices.

What is insulin resistance? (with video)
When a cell loses its responsiveness to insulin, which can happen due to various conditions, it becomes insulin resistant.
Read the ArticleInsulin Sensitivity: The opposite of insulin resistance, insulin sensitivity describes our desired health state: when our cells respond to insulin’s effects as they should.
Insulinemia or Hyperinsulinemia: This means higher than normal insulin levels; it is both a cause and an effect of insulin resistance.
Ketones: When your body needs to burn stored fat for fuel, it converts fat to ketones. Many studies show that using ketones for energy benefits muscle development, cell and organ function, and even brain health. Being in “ketosis” or a “ketogenic state” means that your body is in this ketone-burning mode.

What should I expect to see on my continuous glucose monitor if I’m on a keto diet or in ketogenesis?
What might you see on your continuous glucose monitor if you are on a ketogenic diet? Here are thoughts from metabolic health expert Ben Bikman, PhD.
Read the ArticleLipid: Lipids are a kind of molecule that serves as the structure for many cells, including fats and oils. You may see the term dyslipidemia to refer to an irregular level of one of the cholesterol lipids, high-density lipoprotein (HDL), low-density lipoprotein (LDL), or triglycerides.
Metabolic flexibility: The two main sources of fuel for your cells are glucose and fat. After a typical meal, your body uses glucose (and then glycogen, or stored glucose). As that fuel source runs out (either between meals or during a fast), your body switches to burning fat. The ability to switch between fuel sources is called metabolic flexibility, and it’s something you can train your body to do more efficiently.
Not only is it associated with longevity (PDF), but it can also help you avoid “bonking” or hitting the wall when exercising. That’s because our bodies have a lot more fat than glucose to use as fuel; making that switch quickly can keep our energy up and sustained.
Metabolic fitness: Metabolism is the set of cellular mechanisms that generate energy from our food and environment to power every single cell in the body. When these energy-producing pathways are running smoothly, this represents optimal metabolic fitness.
We talk about metabolic “fitness” instead of “health” because 1) we can work to improve it, and 2) fitness is a continuum; we’re not “healthy” or “unhealthy.” Each improvement is a win.

The ultimate guide to metabolic health
Metabolic health can be improved by consistently making choices that keep glucose levels in a stable and healthy range.
Read the ArticleMetabolic syndrome: Refers to a group of five conditions all related to metabolic health that raise the risk of heart disease, diabetes, stroke, and other problems:
- High fasting blood sugar
- High triglycerides
- Low HDL
- Excess abdominal fat
- High blood pressure
The conditions are interrelated, so people often have more than one. Having three or more is the threshold for metabolic syndrome—estimated to be present in 20-30% of adults globally.
Mitochondria: Often referred to as the energy center of our cells, mitochondria are organelles, or small organs within cells. They have multiple jobs, but one is producing ATP, the energy-storing molecule. Research suggests that mitochondrial dysfunction plays a role in the development of metabolic syndrome through oxidative stress and inflammation.
Mg/dL: Milligrams per deciliter is the standard way of measuring the amount of a substance (glucose) in a fluid (blood). It’s a reflection of concentration rather than the amount.

What should your glucose levels be? Here’s the ultimate guide to healthy blood sugar ranges
Fasting blood sugar levels classify into 3 categories: normal, prediabetes, and diabetes. To be considered “normal,” fasting glucose must be under 100 mg/dl.
Read the ArticleSubcutaneous: The area just under your skin, this is where the measuring probe of the continuous glucose monitor detects glucose in the fluid between your cells.
T1D: Type 1 diabetes is a condition where your body doesn’t make enough insulin to regulate glucose in your blood. It’s thought to be an autoimmune disease in which your body attacks the beta cells in the pancreas. It often appears in children or young adults but can develop at any age.
T2D: Type 2 diabetes is much more common: About 1 in 10 Americans have diabetes, and 90–95% of them have Type 2. Unlike Type 1, Type 2 is wholly preventable. It’s a form of extreme insulin resistance, where chronically elevated insulin causes cells to “numb” to insulin’s effects, so glucose levels can get dangerously high if not carefully regulated.