What does fasting glucose measure?
Glucose is a simple sugar that circulates in your bloodstream and is the primary fuel source for our cells to generate energy. You get it from the food you eat as your body turns carbohydrates into glucose. As crucial as glucose is, more is not better: your body works to keep your circulating glucose at a steady baseline level, using hormones to either shuttle it into cells for energy or into storage, or to retrieve it from storage if you’re running low.
Fasting blood glucose refers to the measurement of that baseline level: your blood glucose levels uninfluenced by a recent meal.
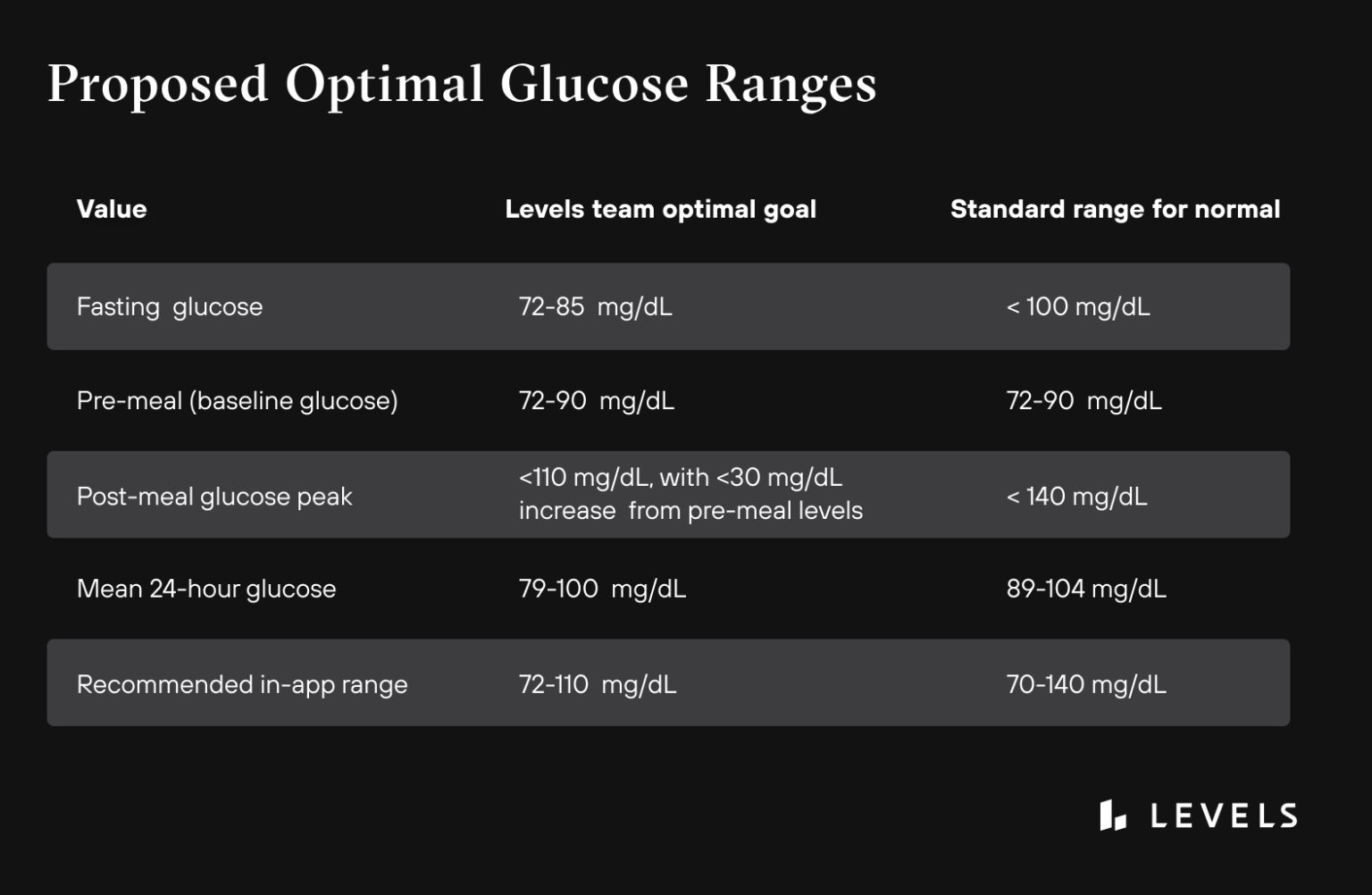
Current medical guidelines recommend a fasting glucose level under 100 mg/dL, but growing evidence suggests normal blood sugar levels are not optimal. Our guidance based on the current state of research and our team of metabolic health experts is that 72-85 mg/dL is a better target for optimal metabolic health. More on that below.
 Want to learn more about your glucose levels?
Want to learn more about your glucose levels?
Levels, the health tech company behind this blog, can help you improve your metabolic health by showing how food and lifestyle impact your blood sugar. Get access to the most advanced continuous glucose monitors (CGM), along with an app that offers personalized guidance so you can build healthy, sustainable habits. Click here to learn more about Levels.
Why should I check fasting glucose?
Fasting glucose is a valuable measurement because it assesses the health of your body’s systems for maintaining its ideal baseline level. If your fasting blood glucose level is high, it’s an indication that something in the process is not working correctly, and that can have serious downstream consequences.
An elevated fasting blood sugar level is related to 8 of the top 10 leading causes of death, and yet many people without a diagnosed metabolic condition pay little attention to it. Most people with a prediabetic amount of glucose don’t even know it.
When you eat and take in excess glucose, your pancreas releases a hormone called insulin, which helps clear it from your bloodstream into cells or storage. But if you consistently spike your glucose levels with high-glycemic foods, for example, your body has to produce large surges of insulin to deal with it. Over time, this can cause insulin resistance—a condition in which your cells become less sensitive to the hormone. Insulin resistance can factor into chronic conditions such as heart disease, kidney disease, diabetes, infertility, and Alzheimer’s disease. Insulin resistance can progress further to Type 2 diabetes mellitus, a condition in which your body is unable to adequately regulate blood sugar.
High blood sugar levels (hyperglycemia) can cause other problems besides insulin resistance. Glucose binds with proteins and lipids in your blood, creating harmful particles called advanced glycation end products (AGEs). AGEs damage the lining of your blood vessels, raising your blood pressure and heightening your risk of heart disease, stroke, and metabolic syndrome. AGEs also interfere with cell signaling, creating oxidative stress and further systemic inflammation. Both oxidative stress and inflammation are fundamental aspects of metabolic illness: they cascade into heart disease, diabetes, obesity, and cancer. The higher your fasting glucose levels, the more AGEs can accumulate, and contribute to your risk for these illnesses.
High fasting glucose can also damage your quality of life in subtler ways. Research suggests that it’s a risk factor for reduced cognitive performance as well as depression and anxiety. It may also be associated with skin issues such as acne, poor sleep, higher stress levels, and sexual dysfunction.
How do I get fasting glucose checked?
To test your fasting plasma glucose, you’ll typically need to refrain from eating for 8-12 hours. This allows the food in your gut to be fully digested so your blood glucose can stabilize. Your blood is then tested using one of the techniques below. Test results are typically reported in milligrams per deciliter of blood (mg/dL) or millimoles per liter of blood (mmol/L).
1. Laboratory blood work
Your healthcare provider or a lab technician draws a blood sample and then tests it. A fasting blood sugar test is usually part of the basic metabolic health blood panel you’d get at your annual physical. You can also request this test directly from a commercial laboratory like Quest Diagnostics or Labcorp.
2. Finger prick testing
Home devices for glucose testing (called glucometers) are available at the pharmacy for $10-$15. You pierce your fingertip with a single-use lancet, place a few drops of blood on a test strip, then insert this strip into the glucometer. The device then instantly reveals your current blood sugar level.
3. Continuous glucose monitor
A continuous glucose monitor (CGM) is a device you wear 24/7 for up to two weeks. It sticks to your skin and painlessly measures your blood glucose in the fluid just below your skin. You can see your levels on a smartphone app, so you can see not only your fasting glucose, but how your body responds to the food you eat, as well as to other lifestyle factors like physical activity. CGMs are prescription devices in the U.S., but Levels helps you get a prescription with an asynchronous healthcare professional consult, and delivers CGMs directly to your door.
What is the optimal range for fasting glucose?
Since the late 90s, major medical groups like the American Diabetes Association (ADA) have recommended the following clinical guidelines for a diagnosis of diabetes:
- Clinically “normal” fasting glucose: Less than 100 mg/dL
- Prediabetes: 100-125 mg/dL
- Diabetes: 126 mg/dL or higher
These standards were based on clinical diabetes studies as well as broad population research showing that the majority of people fall under that 100 mg/dL threshold. But what’s “normal” in the US population may still be unhealthy.
Many subsequent studies have found that people at the upper end of the normal range (i.e. 85-99 mg/dL) still experience serious health consequences, such as heightened stroke, cardiovascular disease, heart attack, and diabetes risk.
Based on this research, Levels suggests that 100 mg/dL still appears too high for healthy metabolism. Instead, we recommend a fasting glucose level of 72-85 mg/dL.
Learn More:

What should your glucose levels be? Here’s the ultimate guide to healthy blood sugar ranges
Fasting blood sugar levels classify into 3 categories: normal, prediabetes, and diabetes. To be considered “normal,” fasting glucose must be under 100 mg/dl.
Read the Article

 Want to learn more about your glucose levels?
Want to learn more about your glucose levels?