A core tenet of metabolic health—the way our bodies make and use energy—is that we require insulin to process blood glucose (or “blood sugar”). It’s the hormone that helps shuttle glucose from the blood into cells. But that’s just one of countless roles played by this essential hormone.
Literally every organ in your body has a sensitive relationship with insulin, and because of that, insulin dysfunction—including insulin resistance—is a root or contributing cause to several chronic conditions, such as heart disease, diabetes, infertility, Alzheimer’s disease, and more. And unfortunately insulin resistance affects more than 133 million Americans, and potentially up to 88% of US adults. So you’d think this vital hormone would be something we test and monitor frequently, but it is not—for a number of reasons. Here, we’ll explore what insulin is, how it impacts your health, why it’s difficult to determine “normal” insulin levels, what insulin levels you should aim for, and how to get tested.
What is insulin?
Insulin is a hormone—a chemical “messenger” that circulates through your bloodstream and triggers physiological events. Produced in your pancreas (a small organ that sits behind your stomach) by specialized β-cells (pronounced “beta cells”), insulin affects every single cell in your body, including your bone, brain, muscle, and skin cells. Of course, given the variety of purposes of these (and other) cells, it’s little surprise that insulin has some distinct actions across these tissues.
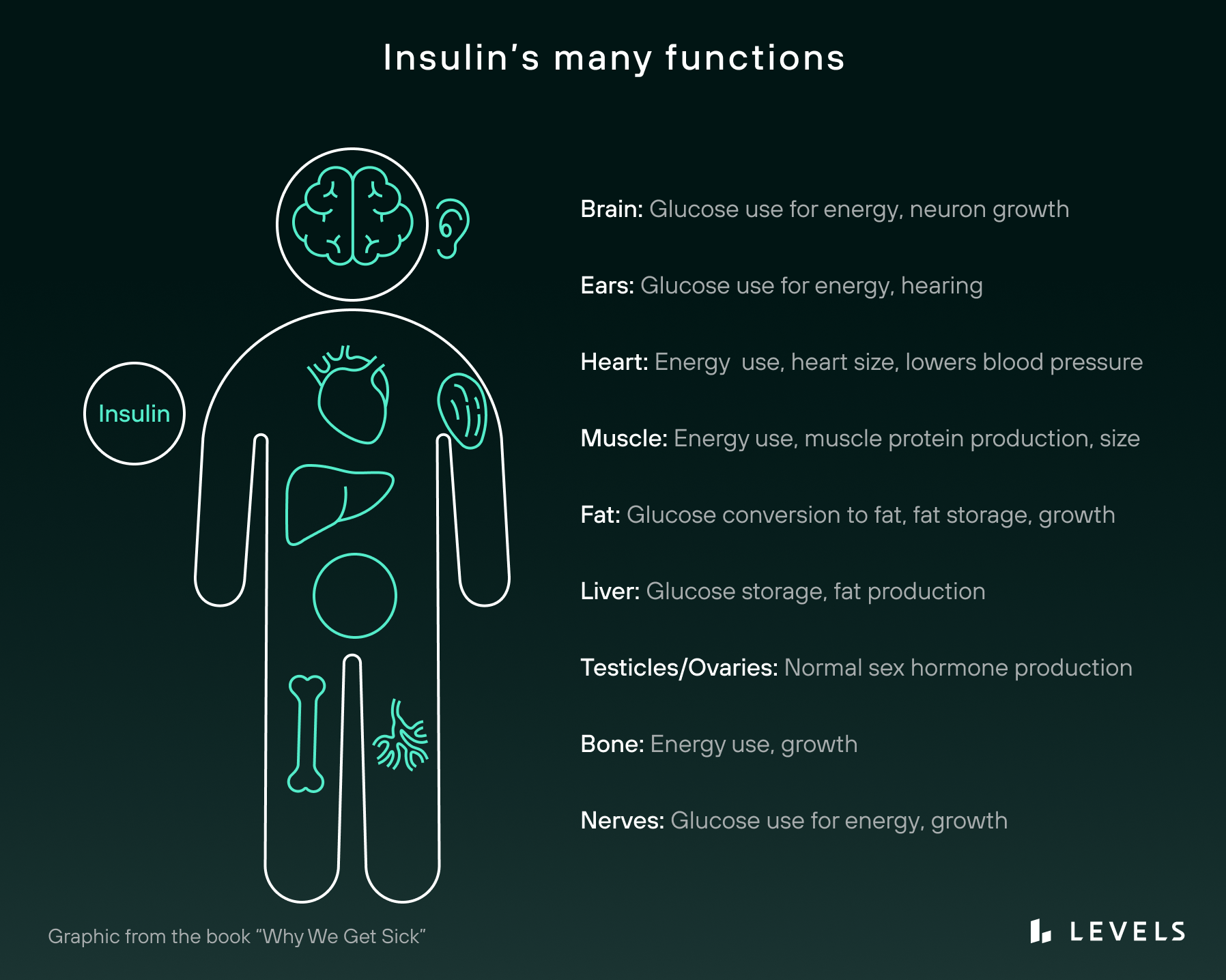
As an anabolic hormone, insulin promotes growth in bones, skeletal muscles, and other tissues. In the brain, there is evidence that it governs cognition, neuronal plasticity, and memory processing. In the kidneys, it helps regulate sodium absorption and homeostasis. And in the liver, insulin helps synthesize alternative energy sources, such as glycogen and fatty acids.
But perhaps the most important function insulin serves is the one it’s best known for: helping your body extract chemical energy from food. When you eat a meal, your digestive tract breaks down carbohydrates and produces, among other things, a simple sugar called glucose. As your blood glucose rises above its baseline, or homeostasis level, your pancreas responds by secreting insulin to help you metabolize this glucose by shuttling it into cells for energy or into storage. This temporarily raises your level of insulin. When the excess glucose has been accounted for, your insulin level falls back to its baseline again.
Insulin and glucose levels are tightly linked in this way because both are necessary to fuel your body on the cellular level. Glucose itself is a main source of chemical energy in the human body, while insulin is the key that unlocks many cells, allowing glucose to enter.
For example, consider a muscle cell. When insulin in your bloodstream comes into contact with that cell, it latches onto the cell’s insulin receptor. This sparks a chemical reaction that brings a special protein to the cell’s surface. This protein is called GLUT4, aka “Glucose Transporter Type 4.” The GLUT4 protein then grabs onto a glucose molecule from your bloodstream and shuttles it back into the cell. There, the cell breaks down the glucose into a more refined form of chemical energy called ATP.
Note that GLUT4 is only one of many glucose transporter proteins that have been discovered—and glucose is not the only energy source that cells can tap into. Even so, the process described above is the dominant way cells obtain chemical energy in the human body. When this process breaks down, the body becomes metabolically unstable with dangerous health consequences.
Due to insulin being overlooked for so long, there is no scientific consensus on optimal insulin levels.
Even in tissues that don’t require insulin to open the cellular doors for glucose, the cells still rely on insulin to tell the cell what to do with the glucose (or any other energy). Unlike the muscle, the liver doesn’t need an insulin signal to pull in glucose from the blood, but that insulin signal is essential to promote the storage of the glucose as glycogen, or even converting the glucose into fats.
Across the muscle, liver, and other tissues, one well-known example of this type of dysfunction is diabetes mellitus. Diabetes is fundamentally a problem of insulin regulation. People with Type 1 diabetes cannot create enough insulin naturally to get glucose into their cells. Without treatment, they may quickly enter a health crisis. Type 2 diabetes, on the other hand, often features excess insulin that becomes less effective. When the body doesn’t respond to insulin properly, glucose levels remain uncontrolled even though insulin levels are chronically elevated. This cascades into many other serious health issues.
Learn more:
Why Do People Without Diabetes Care about Insulin?
Diabetes is perhaps the most prominent insulin-related illness, affecting 37.3 million people (11.3% of the population) in the US. But it is by no means the only one. Many other serious health conditions have been linked to chronically high insulin (hyperinsulinemia) and its close counterpart: insulin resistance.
“Insulin resistance” simply means your cells have stopped responding appropriately to insulin. There are several mechanisms that can drive this condition, including genetics, overnutrition, excess fructose, and excess visceral fat accumulation. Another important one is the chronically elevated insulin, which can result from frequent refined carb consumption.
In the latter case, high glycemic variability and chronically high blood glucose levels (hyperglycemia) cause repeated surges of insulin. As cells are exposed to more and more of the hormone, they become less and less sensitive to it. This “numbing” effect can impact you in diverse ways because almost every cell in your body has insulin receptors. And it can take hold surprisingly quickly. In one study, for instance, researchers forced insulin levels to stay high in a group of 15 healthy people who were previously insulin-sensitive. They became more insulin resistant after just 48 hours of this treatment.

How to reverse prediabetes
Prediabetes is not just a warning diagnosis—it’s a severe metabolic disorder. Fortunately, you can reverse prediabetes with lifestyle and diet changes.
Read the ArticleThe mechanisms driving insulin resistance have to do with the inner workings of living cells. In a skeletal muscle cell, for example, chemical changes (including reduced tyrosine phosphorylation) cause the cell’s insulin receptor to become less adept at receiving insulin molecules and sending messages to other parts of the cell. Meanwhile, GLUT4 may be moved to the cell’s surface less effectively, meaning the cell receives less glucose from the bloodstream. And finally, when glucose is received by the cell, the chemical reactions that convert it to a more refined energy source (such as phosphorylation and oxidation) can also be impaired.
But insulin resistance doesn’t stop there. As your tissues become less sensitive to insulin, your body creates more of it to meet its physiological goals. This elevated insulin level then worsens your insulin resistance, and so on. It’s a vicious circle. And it can culminate in Type 2 diabetes—where the body is so resistant to insulin that it can’t produce enough to maintain homeostasis. At that point, your glucose levels begin to run harmfully high.
This process can take years to unfold. That’s why high insulin levels today may suggest serious health problems in your future—even if your glucose levels are currently within the normal range and you have no diabetes or prediabetes diagnosis. In one study, for instance, high insulin levels preceded high glucose by as much as 13 years. Another study found that hyperinsulinemia can predict glycemic dysfunction 24 years in advance.
Unfortunately, most healthcare providers will not test you for high insulin. Instead, they’ll check for high levels of glucose (and its proxies, like HbA1c). But by the time those downstream symptoms appear, the damage may have already been done by years or decades of hyperinsulinemia.
Here is a short list of other serious health conditions linked to hyperinsulinemia and insulin resistance:
- Metabolic syndrome. A cluster of risk factors all related to insulin resistance, including high glucose, abdominal obesity, high blood pressure (hypertension), low HDL cholesterol, and high triglycerides. People with metabolic syndrome are at higher risk of cardiovascular disease, blood clots, stroke, and other dangerous health events. Metabolic syndrome is closely linked with insulin resistance.
- Heart disease. Insulin may cause or accelerate atherosclerosis by triggering the deposit of unhealthy fats (specifically a dangerous form of LDL cholesterol) into the blood vessels and by thickening the walls of the blood vessels.
- Cancer. Insulin may play a direct role in the formation of cancerous tumors. Insulin resistance is linked with lung cancer, breast cancer, and others.
- Cognitive decline. Insulin resistance is associated with dementia, cognitive dysfunction, and neurodegeneration. Some researchers believe this is due to oxidative stress and other harmful effects of insulin on the brain.
- Reproductive health issues. Insulin resistance has a close and complex relationship with polycystic ovary syndrome (PCOS) and plays a direct role in fertility complications linked with PCOS. Pregnant women with midterm insulin resistance are also at a greater risk for a dangerous complication called preeclampsia. In men, insulin resistance is linked to erectile dysfunction.
- Fatty liver disease. People with insulin resistance are at high risk of developing non-alcoholic fatty liver disease (NAFLD)—a serious and fast-growing illness with potentially deadly ramifications. High levels may play a key role in NAFLD by bringing free fatty acids from the bloodstream into the liver and stimulating fat accumulation.
This sobering (and incomplete) list reveals why insulin levels should be of concern to everyone, whether or not we currently have diabetes: Insulin plays a decisive role in your overall health. By maintaining a safe, controlled insulin level, it may be possible to lower your risk of disease.
What Is A Normal Insulin Level? What Should We Aim For?
Due to insulin being overlooked for so long, there is no scientific consensus on optimal insulin levels. Medical experts take a wide variety of positions on the matter, and a standard reference range has not been established. Generally speaking, we know that lower is better. But where exactly the “danger zone” begins and where insulin becomes harmful are points of contention.
First, consider the reference range published by the physician resource Medscape. It suggests that normal fasting plasma insulin (a common measure of blood insulin levels) should stay under 25 microunits per milliliter (μU/mL). Note, however, that many metabolic health experts consider this range too high. Below, we’ve summarized comments from five Levels advisors—all suggest that fasting insulin should stay below 10 μU/mL.
- Dr. Mark Hyman: Head of Strategy and Innovation at the Cleveland Clinic Center for Functional Medicine, author of 14 best-selling books, focuses on the role of food as medicine.Suggested range: 2–5 μU/mL
- Dom D’Agostino, PhD: Associate Professor at the University of South Florida, leading researcher in neuro implications of keto, runs Keto Nutrition.Suggested range: 2-6 μU/mL
- Dr. David Perlmutter: leading expert in neurodegeneration and metabolic health, author of five best-selling books, including Grain Brain.Suggested range: Less than 8 μU/mL
- Ben Bikman, PhD: Associate Professor at Brigham Young University, leading insulin researcher and author of Why We Get Sick.Suggested range: Less than 10 μU/mL
- Dr. Rob Lustig: Professor emeritus of Pediatrics at UCSF, research and clinical focus on childhood obesity and diabetes, author of four books about the dangers of sugar and processed food.Suggested range: Less than 10 μU/mL
Source: The ultimate guide to understanding your cholesterol panel and metabolic blood tests
Finally, consider what relevant research has to say on the issue. Some of the studies below set out to establish an insulin reference range for a given population. Others simply defined a healthy insulin cutoff for the purpose of studying a related illness. Both can be useful data points:
- A study of 1434 Chinese men found that insulin levels ranged from 1.57 to 16.32 μU/mL, with a median value of 5.79 μU/mL.
- A small study that tested blood samples from 253 people concluded that the upper reference limit of insulin is less than 15 μU/mL.
- A study of 248 Indian participants set the upper limit for normal insulin levels at 17 μU/mL.
- A study found that insulin-resistant obese men are likely to have insulin levels above 74 pmol (12.33 μU/ml).
- A study of 976 Korean adults without diabetes found that people with insulin levels above 10.57 µU/mL were more likely to have metabolic syndrome.
Again, these studies aren’t meant to identify ideal insulin levels—but they can still inform our understanding of a healthy target.
Why Don’t We Know What Optimal Levels of Insulin Are?
Clearly, there is a great deal of confusion about ideal insulin levels, with estimates ranging from 5 to 25 μU/mL—a 5X difference! This ambiguity is due to a confluence of issues.
The first problem is that high insulin was historically viewed as a downstream effect of serious illness, rather than a primary cause. In the last few years, we’ve seen this tide begin to turn. Researchers have published a flurry of papers arguing for insulin’s “pivotal” role in aging, cardiovascular disease, and Type 2 diabetes, as well as obesity, inflammation, and cancer. But the former prevailing wisdom—that elevated insulin doesn’t cause disease—may have impacted research priorities in this area. Why search for a hormone’s “ideal level” if an excess poses little danger?
The second issue is that fasting insulin is entangled with a huge number of other independent factors, like body mass index and body weight, insulin sensitivity, and insulin clearance, as well as diet, exercise, and ethnicity. These factors interact in complex ways, and some (like obesity) are major health risks in their own right. This makes it very difficult to tease apart the variables and identify an ideal insulin level. Is high insulin in an overweight person as harmful as it is in a lean person? How much harm is done by elevated insulin versus the obesity that accompanies it? Should people of different sex and ethnicities have the same insulin target? These are not simple questions for medical researchers.
Ethnicity has proven to be a particularly tricky factor in these analyses. Many studies have found that fasting insulin level varies by ethnicity. For example, this paper found that fasting insulin is higher in post-menopausal Black and Hispanic women than in non-Hispanic White and Asian women. Research has also shown that fasting insulin is higher among Black people than their White and Mexican-American counterparts if the participants are lean—but it is higher among Mexican-American people if they are obese.
These differences can have very real clinical impacts. For instance, the authors of one study found that a race-agnostic threshold for high insulin levels is less reliably linked to metabolic syndrome in Black patients than in others. In other words, Black patients tend to have higher insulin levels by the time they are diagnosed with metabolic syndrome than other populations.
In their efforts to grapple with this complexity, researchers studying health issues like insulin resistance tend to look beyond fasting insulin as a standalone metric. Instead, they have built an array of more complex mathematical scores to assess insulin and its relationship with blood glucose. These include HOMA2-IR, QUICKI, FIRI, and the Matsuda Index. There is ongoing debate and discussion about the relative merits of these approaches, their use alongside other anthropometric data (like BMI and waist circumference), and whether simpler metrics like fasting insulin levels should be substituted.
Finally, a less significant (but still pernicious) issue has been the technical challenge of accurately measuring insulin. In 1996, an American Diabetes Association task force sent identical blood samples to different laboratories for insulin testing. The results were “widely disparate,” raising serious questions about the quality of insulin tests being used in both clinical and research settings. In 2007, another research group found similar results: Insulin tests of identical samples varied by as much as 2X with no explanation.
In an effort to improve insulin assays, researchers and test manufacturers have sought to eliminate several possible culprits. These include:
- Hemolysis: A type of blood sample degradation that can throw off insulin level readings.
- Anti-insulin autoantibodies: In people with autoimmune conditions, antibodies can bind to insulin, rendering it unusable. Some insulin tests can then overestimate the amount of “free insulin” available.
- Cross-reactivity: Historically, insulin tests were sometimes unable to distinguish between insulin and closely related compounds like proinsulin and C-peptide, leading to skewed test results.
While some progress has been made on these fronts, there is still a lack of standardization across insulin tests. The source of this problem remains unclear. As one group of researchers wrote in 2016, “The cause of discrepant results among insulin assays is complex and not yet fully understood.”
This is yet another challenge for researchers who seek to identify optimal insulin levels because it prevents comparison across studies. If two scientific papers use insulin tests from two different manufacturers, the results could mean very different things. In the words of a 2010 study, this makes it “impossible to conduct any quantitative summarization or meta-analysis”—exactly the sort of scientific research that would help us identify the ideal insulin level.
Of course, this doesn’t mean that you shouldn’t test your fasting insulin level. Insulin tests are still legitimate clinical procedures used in the treatment and diagnosis of many illnesses. It simply means that we don’t have as much information as we would like. Hopefully, that will change over the coming years, thanks to the ongoing efforts of academic researchers and test manufacturers.
How Do I Get My Insulin Tested?
As we mentioned above, insulin testing is not typically included as part of routine care. Fortunately, tests are still fairly easy for most people to obtain. You can either request one from your primary care doctor or work directly with a commercial laboratory.
The most common test—a fasting insulin test—requires a basic blood draw and may cost as little as $20. As the name suggests, you’ll need to abstain from food for eight hours before your blood sample is taken. The test results will probably be available in a day or two and will most likely be listed in microunits per milliliter (sometimes written as μU/mL, μIU/mL, or mU/mL).
There is also a slightly more complex test available that paints a clearer picture of your metabolic health. It’s called HOMA-IR—the Homeostatic Model Assessment of Insulin Resistance. This test measures not just your fasting insulin but your fasting glucose. By analyzing these two numbers together, we can see how hard your body is working to control your blood sugar.
Your HOMA-IR test score will be a single number. A score of 1 or less is generally interpreted as the healthy, insulin-sensitive range (though it could also mean low glucose or insulin levels), while a higher score may signify insulin resistance—but how high, exactly, is unclear. Some research groups have put the safe HOMA-IR ceiling at 1.775 in non-diabetic people; others have set it at 1.83; still others have designated a score of 2.5 as the insulin resistance threshold. Note that the original mathematical formula used for HOMA-IR has been largely replaced by a more sophisticated model called HOMA2, so you may see this term in your test results.
Finally, there is a way to infer your insulin sensitivity from a standard cholesterol test. When a doctor tests your lipid profile, the results typically include HDL, LDL, and triglycerides. For a directional approximation of your insulin sensitivity, just divide triglycerides by HDL. If you score above a certain cutoff, this may suggest insulin resistance; researchers have argued that this threshold varies by ethnicity. One group has proposed a ceiling of 2 for non-Hispanic Black people, 2.5 for African American men, and 3 for non-Hispanic White and Mexican-American people.
Note that this approach has limitations. Some research has set the insulin resistance cutoff higher, at 3.5, for this method. Other research has found that the score’s effectiveness in predicting insulin resistance depends on sex. And still other studies have found that its accuracy would improve if other variables—such as sex and waist circumference—were accounted for.
Final Thoughts
Insulin testing can provide valuable health insights. While not yet a routine medical practice, these tests represent a powerful opportunity—both for our healthcare system at large and for conscientious people who want to lower their risk of serious illness and make any necessary lifestyle changes. Although there are open questions about optimal insulin levels, you can still get tested and make an informed judgment with the information available.








