In this new monthly column, the Levels team will highlight a handful of recent studies showing something novel or interesting in metabolic health. We’ll summarize the study, give our perspective on what’s revealed, and link to the original research. For this first installment, we’re looking at a single topic: the risks of elevated glucose in COVID patients.
Establishing the Glucose-COVID Connection Across Multiple Studies
What it Says: This study demonstrates the correlation between high blood sugar and worse COVID outcomes by analyzing data from several other studies looking at this question, including early studies out of Wuhan as well as more recent studies in the US. Researchers examine 10 studies in all, and find that as fasting glucose levels went up, so did severity of COVID in hospitalized patients.
About half of people hospitalized with COVID can develop acute hyperglycemia—that is, their blood sugar goes up as they’re sick with the disease. But these studies also looked at people’s blood sugar when they were admitted to the hospital, and found that patients with elevated levels were three times more likely to die of COVID than those with normal blood sugar. The authors suggest that given the strength of the findings, controlling blood sugar in COVID patients could be crucial to managing the severity of the case.
Why is increased glucose so dangerous for COVID patients? For starters, glucose promotes inflammation and creates compounds called reactive oxygen species (ROS), which may contribute to the “cytokine storm” seen in many severe cases. What glucose values seem to be best? In one of the studies mentioned, fasting glucose on admission of less than 106 mg/dL was associated with significantly fewer complications compared to people with higher levels.
Levels Take: There have been several studies since the first one in June linking high glucose in non-diabetic populations to worse COVID outcomes, but these kind of large scale meta-analyses, in which researchers look at large data sets, are especially helpful. This study shows that elevated fasting glucose levels at hospital admission are related to higher mortality from COVID, regardless of whether the patient had been diagnosed with diabetes. Given that, we agree with the paper’s conclusion: “The need for timely recognition and management of blood glucose levels should be emphasized in COVID-19 disease.” It’s time that we put resources into helping people improve blood sugar on a large scale.
Seeing the Effect on a Large Sample
What it Says: This recent study from Spain also makes the connection between high glucose levels and worse COVID outcomes, independent of diabetes diagnosis. What’s powerful is the sample size: The researchers look at the records of more than 11,000 people; many of the previous studies had sample sizes under 1,000. This gives us even more confidence in this correlation.
The study also discusses inflammation, suggesting “early correction of hyperglycemia in the course of COVID-19 could result in a decrease in the release of inflammatory cytokines… resulting in better outcomes.” The authors outline other reasons, beyond inflammation, that high blood sugar relates to worse COVID outcomes, and why hyperglycemia often gets worse in patients fighting COVID.
First, SARS-CoV-2 can infect pancreas cells via ACE2 receptors, impairing the organ’s ability to create insulin, which helps regulate glucose. There’s also a relationship between hypoxia—not getting enough oxygen, a common symptom of COVID—and impaired glucose metabolism. Normally, glucose processing produces ATP, our cell’s form of energy. In low-oxygen conditions, glucose metabolizes into lactate, which produces less ATP. Hypoxia and low ATP levels mean higher circulating blood lactate and a compound called lactate dehydrogenase (LDH). And elevated LDH has also been associated with higher COVID mortality. So far only one small study has looked at using oxygen to correct this anaerobic glucose metabolism at the early stages of COVID, but it’s an area that deserves more research.
The study shows that of people admitted to the hospital with high glucose levels (between 140-180 mg/dL), only 38 percent had a prior diabetes diagnosis. This suggests that there may be a significant amount of undiagnosed diabetes in the population, or that the virus worsens glucose control. In terms of death rates in the hospital, diabetes diagnosis didn’t matter: high glucose at admission equaled higher mortality.
Levels Take: This research is piling on evidence of the dangers of high blood sugar for COVID patients—but it’s a big pile of evidence. And it underscores 1) how vital it is that hospitals screen patients for hyperglycemia at admission and treat it early; and 2) how important it is to control your metabolic health, all the time. We know that only 12 percent of people are metabolically healthy—that leaves a big potential pool of people that could suffer unnecessary additional risk if they’re unlucky enough to get sick with COVID.
Finally, we agree with the authors’ suggestion that providing glucose monitoring to patients who are asked to stay at home during the early stages of infection would be extremely valuable given what we now know about COVID and metabolic health.
Creating a Way to Manage Glucose in Hospitalized Patients
The Study: Managing Hyperglycemia in the COVID-19 Inflammatory Storm
What it Says: This study from the University of Michigan looks at COVID patients in Michigan to better understand why high blood sugar seems to worsen outcomes, and what can be done about it. The study notes that a pattern of severe high blood sugar was seen in a large proportion of patients—not just those with prior diagnosis of diabetes, prediabetes, or severe obesity—and that many of these patients rapidly worsened.
Building on previous research, the authors believe the low-grade, persistent inflammation associated with hyperglycemia “promotes fertile ground for the virus’ inflammatory surge, resulting in severe insulin resistance and severe hyperglycemia.” This creates a damaging cycle: People with high blood sugar are more likely to get more seriously ill, which further raises their blood sugar. The researchers also created a protocol for assessing a patients’ hyperglycemia and treating it with insulin while they are hospitalized, aiming for a glucose goal of 150-180 mg/dL in most patients.
Levels Take: We chose to highlight this research because it’s an interventional study, meaning the authors tested a glucose management protocol on patients, rather than just reviewing existing data. And it adds to the literature about the mechanisms behind the impact of elevated glucose on COVID. Finally, the treatment protocol is an actionable, potentially life-saving aspect of this research: It helps nurses treat hyperglycemic patients while keeping themselves safer. This article goes deeper into that part of the study.
Uncovering a Surprise: Low Glucose Can Also Cause Problems
What it Says: This study out of Wuhan, China correlates the blood glucose levels of 293 non-diabetic COVID patients with the severity of their illness, and finds a J-shaped curve. That means that not only were people with the highest glucose most likely to have negative outcomes, but people with low fasting glucose (85 mg/dL and below) also fared worse than those with fasting glucose in the higher end of the normal range (85-93 mg/dL).
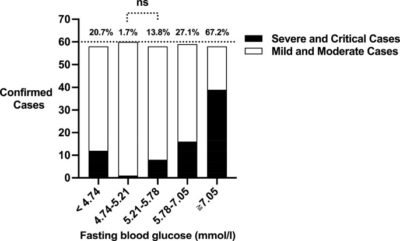
The J-shaped curve between glucose levels and COVID severity.
While this study doesn’t specifically investigate why lower glucose can worsen the disease, the authors speculate based on other research that it’s an energy shortage problem. COVID replication consumes a lot of the body’s ATP, which is made by metabolizing glucose. So if you already have low glucose, and therefore low ATP, and then COVID consumes even more ATP, your body simply doesn’t have enough energy left to mount a robust immune response. Your body also needs glucose to generate antioxidants like glutathione, so low glucose could also impair your antioxidant defenses.
Levels Take: Two things strike us about this study. First, if the finding holds up under further research, it’s fascinating that low blood sugar would lead to worse outcomes (though the proposed mechanism around ATP makes sense: the body needs energy to fight off the disease). It’s a reminder of just how fundamental metabolic processes are. Second, it’s indicative of how much we have yet to learn about COVID and how it interacts with the body. That the story of high glucose and COVID is so clear already underscores the strength of the connection, but as researchers dig further into data, we will surely find more unexpected results like this one.