Most conversation about blood sugar happens in the context of diabetes—a condition characterized by chronically high glucose levels (AKA blood sugar). However, it turns out that glucose dynamics affect everyone’s health.
When blood sugar is erratic, you can experience poor energy and focus in the short term and develop serious health conditions in time, no matter how thin, fit, or seemingly healthy you are.
Your blood sugar levels contribute to common health concerns like weight gain, hormonal issues, and mental health, as well as chronic conditions such as Alzheimer’s disease and cardiovascular risk.
Understanding why blood sugar changes and why that matters is core to your daily experience and long-term health. It’s also vital to our health as a society.
Blood sugar problems are pervasive—more than a third of US adults have prediabetes, and 80% don’t know it. Eight of the top 10 leading causes of death are tied to high blood sugar and its consequences.
The good news is that you can change your blood sugar levels. In fact, this critical health lever is largely within your control, changeable with simple tweaks to your daily habits. By adjusting behaviors like diet, exercise, stress levels, and sleep, you can meaningfully move the needle on your blood sugar and take control of your health.
Read on to learn what blood sugar is, the many aspects of health it influences, how to change it, and how to measure your levels.
What is blood sugar?
Blood sugar, or glucose, is one of the primary energy sources powering cells in your body. When you eat foods with carbohydrates, your body converts them into glucose as they break down, causing your blood sugar level to rise.
Eating will nearly always cause a gradual rise in blood sugar, as most foods—even whole vegetables—have some level of carbs. That’s normal and healthy. Your body has processes for getting your glucose back to its baseline.
However, some meals can produce a “spike,” or dramatic increase in blood sugar levels. The types and quantities of foods we eat cause different degrees of spike, and how we react to food varies among people. And today, we’re bombarded with many times more sugar and refined carbohydrates (the type most likely to spike blood sugar) than our ancestors ever were; we consume nearly 10x more sugar per day than we did 200 years ago.
Lifestyle factors like exercise, sleep, and stress also impact blood sugar response. Poor sleep, for instance, can lead to higher blood sugar spikes the next day. Exercise after eating can blunt rises.
Big blood sugar spikes and subsequent crashes represent a fueling system gone awry. When spikes happen repeatedly, they can have serious impacts on health. These consequences are partly due to how glucose spikes impact insulin and can create insulin resistance.
What is insulin resistance?
When glucose levels rise, your body produces a hormone called insulin, which helps process glucose and shuttle it from the blood into the cells. Producing insulin is normal, but when glucose spikes are too big or too frequent, they cause more and more insulin production. This eventually leads to cells becoming less responsive to insulin, a state known as insulin resistance. In response, the body produces more insulin to deal with the glucose, which worsens insulin resistance, eventually leading to chronically high blood sugar. Insulin resistance is at the root of many health problems stemming from poor blood sugar regulation.
Why do people associate blood sugar with diabetes?
The primary condition most associated with blood sugar and insulin is diabetes. While this is true for Type 1 and Type 2 diabetes, they are otherwise different conditions.
Type 1 diabetes is an autoimmune condition in which the body can’t produce insulin. People with Type 1 must give themselves insulin to manage their blood glucose levels throughout the day.
Type 2 diabetes and its precursor, prediabetes, are almost entirely preventable. Prediabetes and Type 2 diabetes happen when insulin resistance is so advanced that blood sugar remains chronically high. About 95% of all diabetes is Type 2, and it’s now more common in children than ever before. Over a third of adults in the US have prediabetes, and 80% don’t even know they have it.
Unlike Type 1, Type 2 is largely reversible through lifestyle choices that help keep blood sugar stable. This reduces insulin resistance, allowing your blood sugar levels to decrease over time.
If you haven’t been diagnosed with diabetes, chances are you haven’t learned about these processes. But everyone should take insulin resistance seriously before it becomes so severe that it is labeled prediabetes or Type 2 Diabetes. Glucose spikes and the insulin resistance they create can harm your health long before you’re diagnosed with one of these metabolic conditions. Prevention is easier than reversal.
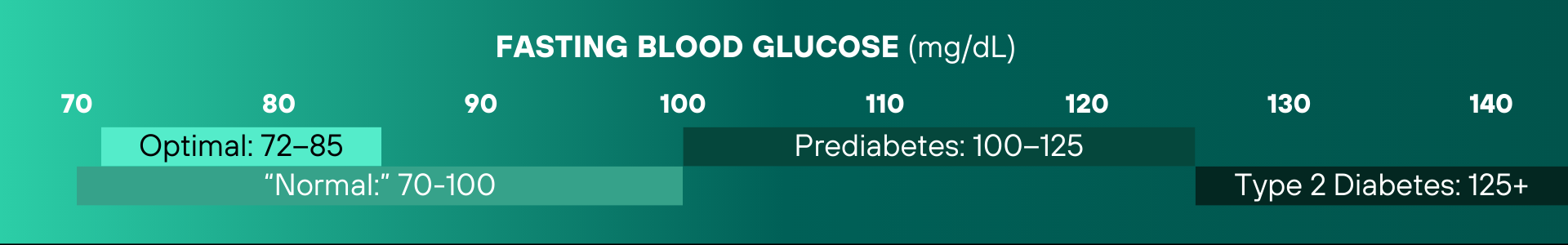
Blood sugar levels exist on a spectrum. It’s important to remember that cutoffs are necessary for diagnostics but are, in a sense, arbitrary. Being at the top end of a range is worse for your health than being at the low end.
How does blood sugar impact health?
Since glucose is fuel for your cells, dysregulated glucose can impair how your cells work throughout your body, driving dysfunction in your veins, brain, organs, muscles, and more. And the effects of that cellular damage cause everything from subtle differences in how we feel to our overall mortality risk.
Blood sugar impacts your daily experience
There are many everyday impacts of blood sugar dysregulation. When blood sugar is high, it can lead to fatigue, brain fog, cravings, and even bad skin.
If you’ve had a sugar high or sugar crash, experienced an afternoon slump, or felt bad when you’ve gone a long time without eating, these are all related to having blood sugar levels that are too high or too low.
However, when blood sugar is stable, our energy levels are higher, our skin is clearer, we have more mental clarity and better memory, and we are less susceptible to cravings or crashes that throw off our eating habits.
Blood sugar matters for everyday health concerns
Blood sugar is also relevant to many health issues people manage regularly.
For example, when your blood sugar (and insulin) levels are consistently high, your body begins to convert excess glucose into fat, which can lead to weight gain. Also, insulin prevents fat burning, so high insulin levels make it harder to lose that extra weight.
Blood sugar also matters when dealing with hormonal dysfunction. PCOS, menopause, female and male infertility, and the entire process of the pregnancy journey—from preconception nutrition through postpartum and breastfeeding—can be significantly affected by blood sugar control.
Glucose also plays a role in mental health. Depression and anxiety have both been linked to poor blood sugar control.
Blood sugar affects your risk of chronic health conditions
Repeated blood sugar spikes cause damage in your cells that, over time, can contribute to developing chronic conditions. Similarly, insulin plays crucial roles in several processes, so when it’s dysregulated because of insulin resistance, it can increase your risk of other diseases. Here are just a few of the long-term health problems related to blood sugar:
- Type 2 diabetes is the condition of chronically high glucose levels and is itself the eighth leading cause of death; its complications also contribute to others, such as cardiovascular disease.
- Dementia and Alzheimer’s disease are so associated with poor metabolic health that the latter is commonly referred to as Type 3 diabetes.
- The risk of heart disease is worsened by insulin resistance and high glucose, which can damage blood vessels.
- Certain types of cancer are also more common among people with glucose dysregulation, including breast and prostate cancers.
Learn more:
What can I do to maintain healthy blood sugar?
Healthy glucose levels are largely in your control through your lifestyle choices around diet, exercise, sleep, and stress. That said, it can still be challenging in our modern environment, saturated with hidden sugars and toxins. The good news: these don’t have to be massive changes like going vegan or training for a marathon. Simple changes go a long way when it comes to metabolic health. Here are four key levers of blood sugar control.
Eat foods that keep blood sugar stable
The most important thing you can do is eat foods that don’t cause sharp rises, specifically focusing on nutrient-dense, whole foods, and avoid foods that spike your blood sugar, such as processed foods. It’s essential to consider your choice of carbohydrates and stick to carbs that your body can process slowly, such as vegetables with lots of fiber.
Change how you eat your food
While what you eat is essential, research demonstrates that how you eat also matters. For example, whether you eat carbohydrates alone or with proteins or fats, the order in which you eat your food and the time of day you eat all make a difference in how blood sugar rises.
Exercise regularly
Exercise has a profound impact on blood sugar, no matter the intensity. Studies show that simply walking after a meal can blunt a blood sugar rise. Meanwhile, Zone 2 cardio and more intense exercise like HIIT or weight training helps your body build the ability to process glucose better. The bottom line: choose the activity that works best for you and move every day.
Prioritize healthy sleep and stress levels
Research suggests that getting less than six hours per night impairs glucose metabolism and increases insulin. Not only is the amount of sleep relevant, but sleep quality makes a big difference.
Stress can also lead to higher glucose levels through the relationship between stress hormones like cortisol and adrenaline on glucose and insulin.
How do I check my blood sugar levels?
Blood sugar is also one of the few biomarkers in our body that we can easily measure ourselves. Monitoring blood sugar can be incredibly useful in determining what inputs affect you in real time. Perhaps you are more impacted by stress than you think, or certain carbs cause spikes while others don’t. Knowing your levels lets you have actual data to see which behaviors or choices impact your health.
You can assess your blood sugar in a few ways. The most common practice is checking metabolic health metrics in routine bloodwork at your annual physical. However, that just gives a single snapshot in time, so it’s a potential long-term indicator of your overall glucose picture. You can also check your blood sugar using finger-prick tests sold at the pharmacy; this is how many people with diabetes manage their levels. Finally, you can wear a continuous glucose monitor (CGM), a small device stuck to your arm or abdomen for up to two weeks that constantly tracks your blood sugar levels.
The Levels app pairs with CGMs to analyze your blood sugar data and provide insights and recommendations. It also helps you track long-term trends and develop healthy habits based on your data.
What are healthy blood sugar levels?
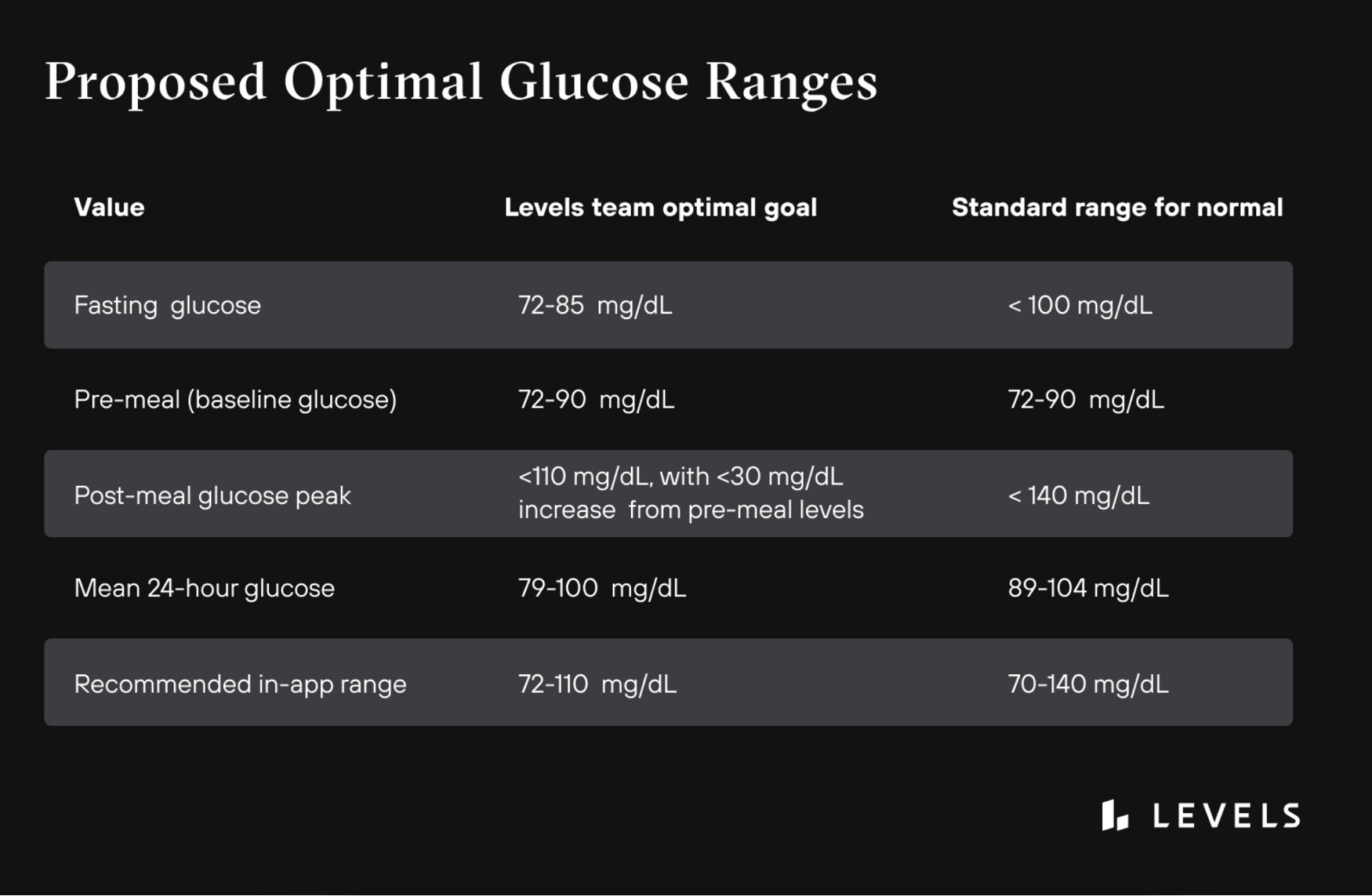
There are a few key measurements important for measuring blood sugar. At your annual physical, you’ll be tested for fasting glucose, which is your blood sugar unaffected by a recent meal. This is important, but it can look healthy even as dysfunction develops in the background. Post-meal glucose is a good measure of how your body’s systems for dealing with blood sugar are functioning.
It’s important to know that the standards for “normal” levels don’t factor in a preventative approach, and research shows that even being at the high end of normal can increase your health risk. Therefore, we recommend the following optimal levels:
Conclusion
Blood sugar is a critical health metric most of us don’t think enough about, even as it can silently wreak havoc on our day and our long-term well-being. However, it’s also one of the most controllable factors, easy to influence with simple, day-to-day choices. Just by being more mindful of how what you eat and do impact your blood sugar, you can do a lot to improve your life and health.
 Interested in how CGM can help you track your glucose levels?
Interested in how CGM can help you track your glucose levels?
Levels, the health tech company behind this blog, helps people improve their metabolic health by showing how food and lifestyle impact your blood sugar, using continuous glucose monitoring (CGM), along with an app that offers personalized guidance and helps you build healthy habits. Click here to learn more about Levels.


 Interested in how CGM can help you track your glucose levels?
Interested in how CGM can help you track your glucose levels?






