Getting a test result for fasting blood sugar—the amount of glucose in your blood independent of a recent meal—that falls into the “normal range” doesn’t necessarily equate to a clean bill of health and wellness. But what are normal glucose levels? Some research suggests that today’s blood glucose standards are not exactly optimal. New data collected from continuous glucose monitors in healthy people over the past several years has begun to reveal normal glucose fluctuations in people without diabetes, but we still have an incomplete picture and don’t fully understand the clinical significance of those fluctuations. What we can see is that meaningful risk exists within the current range of normal blood sugar levels.
And since diabetes affects more than 11 percent of the US population (37 million people), and as much as a third of the US population has prediabetes, a change in these standards could have implications for public health by preventing or reducing illness in people with levels in the upper range of today’s thresholds. Additionally, high blood sugar levels are associated with 8 of the 10 leading causes of death, and metabolic dysfunction can have short-term impact on quality of life. So understanding our blood sugar targets could help all of us be healthier, avoid various medical conditions, and feel better.
Read on to learn what we know, where we still have questions, and what Levels metabolic health expert advisors believe should be our targets.
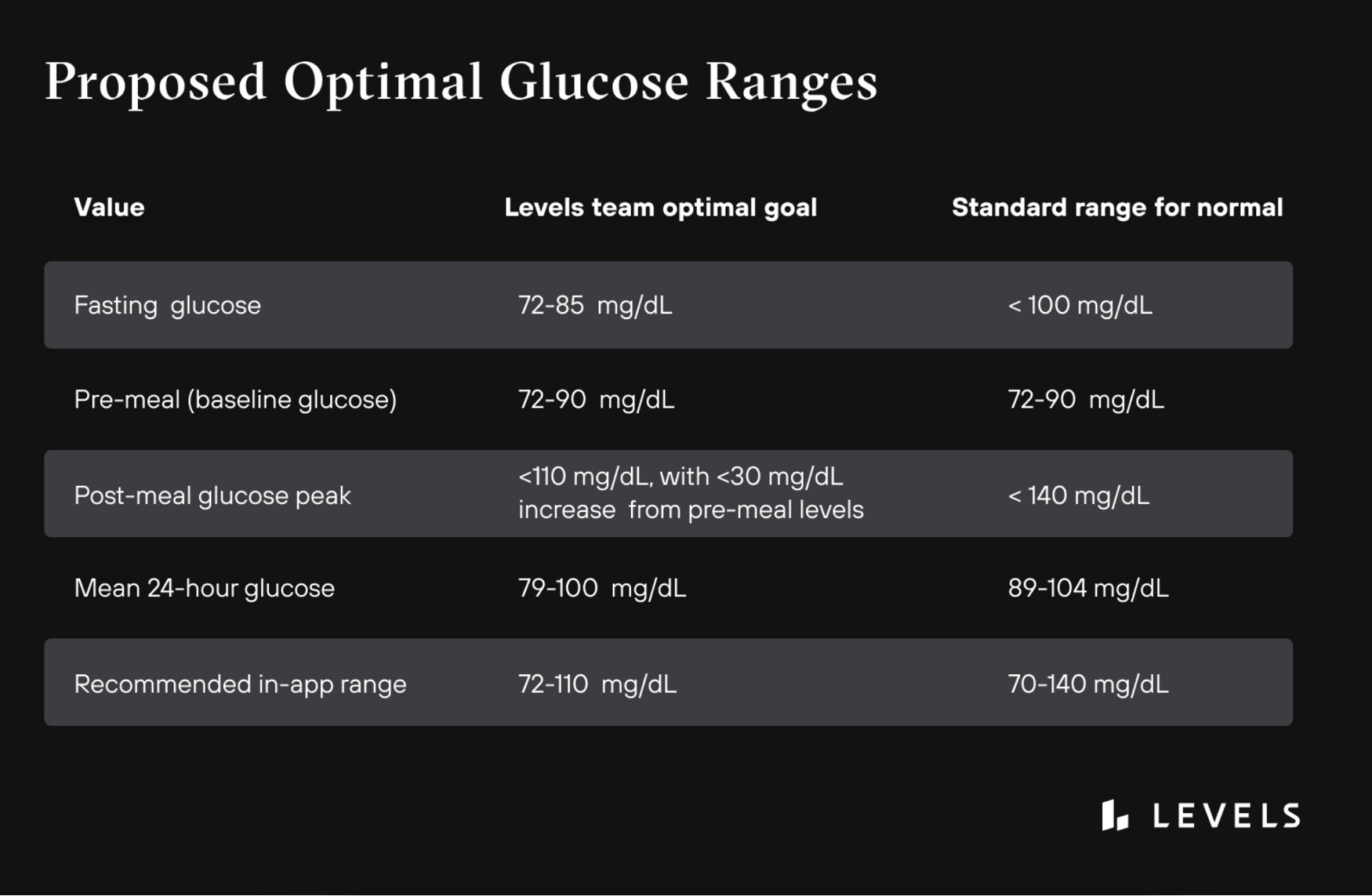
Tl;dr: Levels recommended guidelines for optimal glucose
Where do the current glucose guidelines come from?
An expert committee convened by the American Diabetes Association in 2003 determined the blood glucose guidelines that doctors still follow today. Using numerous research studies, the ADA committee determined fasting and post-meal glucose thresholds for diagnosing diabetes. In addition, they established the upper limits of the normal range linked to a sharp rise in the incidence of diabetic retinopathy, an eye disease caused by high blood glucose that can lead to blindness.
Although the committee didn’t determine a lower threshold, today, normal fasting blood glucose levels are generally considered between 70 and 100 mg/dL, with postprandial blood glucose levels not jumping higher than 140 mg/dL. The committee determined that staying within these ranges would prevent the onset of diabetic retinopathy.
For diagnosing Type 2 diabetes, they determined people with a fasting blood sugar range between 110-125 mg/dL have prediabetes, and those whose levels equal or exceed 126 mg/dL have diabetes. The benchmarks are still used widely today. In addition to using the A1c test (a blood test that shows your average blood sugar level for the past 2–3 months by measuring the percentage of hemoglobin with blood sugar attached), doctors use these fasting blood glucose thresholds to make clinical diagnoses and lifestyle recommendations, plus medication, diabetes care, and treatment plan decisions.
We should also note that hyperglycemia is only one marker and risk factor of metabolic dysfunction, and it’s an imperfect one in many ways. We also need to pay attention to insulin, the hormone that (among many other jobs) helps shuttle glucose out of the blood and into cells. As you take in more glucose, your body produces more insulin. So ever-increasing levels of insulin can actually mask glucose problems for as long as a decade or more before insulin can’t do its job anymore, and you finally see high glucose in a blood sugar test. Ideally, you want to test insulin alongside glucose, but unfortunately, the test isn’t standard yet in most physicals. Read more about insulin and testing here.
 Want to learn more about your glucose levels?
Want to learn more about your glucose levels?
Levels, the health tech company behind this blog, can help you improve your metabolic health by showing how food and lifestyle impact your blood sugar. Get access to the most advanced continuous glucose monitors (CGM), along with an app that offers personalized guidance so you can build healthy, sustainable habits. Click here to learn more about Levels.
What do we know about glucose levels in people without diabetes?
Some healthcare providers and researchers feel these levels could be lowered in order to identify more people at risk of diabetes. The major difference here is in the classification of what are normal blood glucose levels—meaning the lack of diagnosed disease—versus what is optimal for long-term health.
“The word normal doesn’t mean optimal,” says Dr. Robert Lustig, Professor emeritus of Pediatrics, Division of Endocrinology at the University of California, San Francisco (UCSF). Lustig thinks that diabetes levels ought to be lower than they are today for optimal health. He says that the so-called normal levels were determined by studying people who probably already had some form of metabolic disease but didn’t know it.
Research has shown that most Americans today have at least one marker of metabolic syndrome, but many don’t know it. The prevalence of disease in the population makes it difficult to make assumptions about health. In his view, lower blood glucose is better. “Optimal blood glucose is as low as possible until you have [hypoglycemic] symptoms,” he says.
Continuous blood glucose monitoring, which has grown in availability over the past several years, is helping researchers drill down into this issue by delivering much more data than they had in the past. Whereas earlier studies relied on in-lab blood draws to get fasting data, continuous glucose monitors (CGMs), which allow for 24/7 tracking of blood sugar in study participants, create the opportunity for researchers to get a clearer picture of what happens to blood sugar in people without diabetes as they go about their day. This allows us to capture not just fasting glucose but also glycemic variability, or how much glucose levels change after a meal or other events (physical activity, sleep, etc), which may be a better indicator of metabolic health.
Unfortunately, there are still very few studies like this. (Levels is currently running a study of up to 50,000 people to learn a lot more.) So it’s vital to point out that the clinical significance of the blood glucose fluctuations captured by CGM is still unknown, and there are no specific recommendations regarding the average levels over a 24-hour period using CGM.
In short, we don’t fully know what normal looks like in a general population. But we can glean some insights from the studies that have been done. For example, a 2007 study in Germany looked at 21 healthy volunteers between the ages of 18 and 35 with a normal BMI. They wore CGMs as they ate standardized meals for 48 hours and then returned home and at regular meals for another 48 hours. The results from those regular eating days showed that they spent 80 percent of the time in the range of 59-100 mg/dL and only 20 percent between 100-140 mg/dL. The study was small and short, but the results suggested that glucose ranges in young healthy people tend to skew lower than the current normal ranges.
Learn more:
What do we know about post-meal glucose targets?
Blood glucose naturally rises after you eat as your body converts carbohydrates to glucose—these fluctuations are called glycemic variability. Frequent post-meal rises that look like steep mountains—or spikes—also lead to sharp falls, often below fasting levels. This pattern is associated with a range of problems like weakened glucose control over time, obesity, diabetes, cardiovascular disease, heart attack, and impaired exercise and cognitive performance. Over time, it drives insulin resistance, which is at the heart of metabolic syndrome and a driver of many chronic conditions.
When it comes to post-meal glucose targets, the International Diabetes Federation (IDF) suggests people without diabetes should reach no higher than 140 mg/dL after meals, and glucose should return to pre-meal levels within 2-3 hours. Some recent studies show current targets may be on the higher side. The research is limited, so we don’t want to over-rely on these results, but a couple of studies over the past several years have hinted at lower spikes in healthy populations.
- One study from 2009 enrolled more than 400 healthy subjects in China and had them track blood glucose continuously for three days. Their average levels one hour after eating were 121-123 mg/dL, and their mean fasting glucose was 86 mg/dL.
- In another study from 2019 in the US, researchers fitted healthy, non-obese children and adults with CGMs for up to 10 days. They found that across people, a median of 89% of glucose readings fell between 70 and 120mg/dL.
Why current fasting glucose targets may be too high
One challenge with the current guidelines is that glycemic control is a spectrum, and the range considered healthy is very broad. Multiple research studies show that as fasting glucose increases, there is an increased risk of health problems like diabetes and heart disease—even if it stays within the normal range.
- In one study, men whose fasting blood sugar level was greater than 85 mg/dL had a significantly higher mortality rate from cardiovascular diseases than men with blood sugars less than 85 mg/dL.
- In another study, both men and women with fasting glucose levels in the high normal range (95-99 mg/dL) had significantly increased cardiovascular disease risk than people whose levels remained below 80 mg/dL.
- The upper level of normal has also been associated with an increased risk of developing diabetes. One study showed that children with fasting glucose levels 86-99 mg/dL had more than double the risk of developing prediabetes and Type 2 diabetes as adults when compared with children whose levels were less than 86 mg/dL.
- Another study showed that adults with fasting glucose levels between 91-99 mg/dL had a two-fold increase in Type 2 diabetes risk compared to those with levels less than 83 mg/dL.
Another key point is that metabolic dysfunction develops slowly over time, not all at once. By the time your fasting or post-meal average glucose levels start creeping to the high end of normal, you may already have advanced insulin resistance since your pancreas can keep pumping out more insulin to keep glucose levels “normal.” By taking note of high or increasing levels, even in the normal range, you can take actions to reduce them before you cross the threshold into full-blown disease.
What does the Levels glucose study show?
Levels is running an independent review board (IRB)-approved study that uses the aggregate anonymized glucose data from our members to better understand glucose patterns among people without diagnosed diabetes. The study began in 2022 and has had more than 35,000 participants. Here are some highlights from what we’ve seen in our data so far.
Post-Meal Glucose Levels
Breakfast
- Average Glucose for 2 hours post meal = 105.96 mg/dL
- Glucose Delta: 20.69 mg/dL (difference between highest and lowest glucose reading during the zone)
Lunch
- Average Glucose for 2 hours post meal = 107.8 mg/dL
- Glucose Delta: 36.8 mg/dL
Dinner
- Average Glucose for 2 hours post meal =107.18 mg/dL
- Glucose Delta: 28.24 mg/dL
Waking Glucose
Waking glucose approximates your fasting glucose levels, a measure of your blood sugar levels unaffected by a recent meal. It looks at the average in the hour before waking to avoid being impacted by the dawn effect, a natural rising of blood sugar when you wake up.
Mean waking glucose: 107 ± 16.47 mg/dL
Dawn effect: Levels members experience an average dawn effect of 7.05 ± 9.95 mg/dL (Grouped by member)
Time in Range
This describes the amount of time members stayed between 70–140 mg/dL for an average of the day.
People spend an average of 64.58% of the day (± 31.35%) under 110 mg/dL
Participants spent ~80% of the time between glucose values 59-100 mg/dL and 20% of the time between 100-140 mg/dL.
Daily Glucose Metrics
Mean 24-hour glucose levels were 106 mg/dL (± 19 mg/dL).
- Maximum daily glucose levels were an average of 149.68 mg/dL (± 22.08 mg/dL).
- Out of the 35,407 participants, 7.2% of members averaged a diabetic response to lifestyle activities of a max glucose greater than 180 mg/dL
A note about individuality
One of the reasons additional large-scale research in undiagnosed people is so important is that metabolic health can be highly individual. A food that generates a sharp blood sugar response for you may not spike me at all. Sleep and stress also play key roles in our glucose movement. In addition, our metabolic health is influenced by our genetics, our microbiome, and the rest of our overall health.
So it’s important to take guidelines like those below as targets that help you maintain long-term healthy trends. Metabolic health is not determined by a single event.
What are optimal glucose levels?
Based on our reading of this research, as well as the guidance of our metabolic health expert advisors, we suggest you aim for slightly more conservative values in your glucose.
Fasting Glucose
What is it: This is your blood sugar unaffected by a meal, your baseline.
Why does it matter: It’s a snapshot in time, but if it is high, it’s a good indication that some metabolic dysfunction is present. “Once fasting glucose rises over 100 mg/dL, metabolic syndrome is in full force. A fasting glucose of 90 mg/dL is already questionable,” says Lustig.
How do you measure it: Typically measured by a blood sample at your annual physical. You can also check it yourself with a finger-stick glucometer from the drugstore; just be sure you are completely fasted. A CGM paired with software like Levels that tracks meals will give you the best view, as you can see how long it has been since your last meal and observe your fasting ranges over time.
Target range: Aim for the 70s-low 80s mg/dL.
Postprandial Glucose
What is it: Your blood sugar in a two-hour window after you eat.
Why does it matter: How your body responds to a glucose load, like carbs in a meal, reveals how your metabolic machinery is working. Ideally, your body is able to clear the glucose quickly, without a significant rise, and return to baseline. “Not all people with prediabetes have high fasting glucose, so we want to look at the full dynamic range, including after meals,” says Dr. Sara Gottfried, Director of Precision Medicine at the Marcus Institute of Integrative Health-Jefferson Health and Levels advisor.
How do you measure it: In a doctor’s office, this is measured through an oral glucose tolerance test, or OGTT, in which you consume a sugary drink and get blood draws at regular intervals. A simpler, more comprehensive way to see it is with a CGM, which allows you to see your response to all meals, so you aren’t reliant on a single data point. Your glucose response will vary considerably depending on what you eat and other factors like time of day, stress, and sleep.
Target range: Aim for glucose levels to stay under ~110–115 mg/dL at any time point after meals.
Conclusion
While there is a lot we don’t yet know about what constitutes normal blood sugar for the broad population, we know a lot about the consequences of metabolic dysfunction. We also know that metabolic health is largely in our control, so catching any developing issues early gives you a chance to course correct through diet and lifestyle changes. Pay attention to your blood sugar, and aim to keep it stable and healthy.

 Want to learn more about your glucose levels?
Want to learn more about your glucose levels?







