Terry Wahls, MD, was in medical school when the nerve pain started: sudden bursts of electrical pain shooting down her face to her jaw for just a moment. Five years later, she experienced dim vision in her left eye while roller skiing after work. She saw a neurologist and an ophthalmologist and was told she had autonomic dysfunction of the retinal blood flow. And to stop pushing herself so hard when she worked out.
Over the following decade, the electrical pains would become more frequent, severe, and difficult to turn off. Thirteen years after Wahl’s first symptoms began, she was diagnosed with multiple sclerosis (MS), an autoimmune disease that causes a person’s immune system to attack myelin—the protective sheath that coats nerves. Without it, communication between the brain and the rest of the body breaks down.
Despite seeing the best physicians at one of the best MS clinics in the country, three years later, Wahls needed a tilt/recline wheelchair. That was when she asked herself if she was doing all she could to control her disease.
A clinical professor of medicine a the University of Iowa, Wahls knew how to read the research. At first, she focused on the animal studies used to develop new drugs. Then she decided to begin looking at studies investigating nutraceuticals that are nutritional supplements in the setting of progressive neurological disorders. As she read the studies, an idea began to cement.
“It appeared to me that the root cause was mitochondria, that they couldn’t make enough energy to maintain healthy brain tissue,” she says, referring to the structures that drive cells’ metabolic processes. The lack of adequate energy leads to the slow deterioration of the brain cells and the onset of Alzheimer’s, Parkinson’s, and other progressive neurological disorders. The same process was likely occurring in progressive multiple sclerosis. “So, I concocted a supplement regimen that focused on supporting mitochondrial function.”
The supplement cocktail reduced the severity of her fatigue but did not completely resolve it.
Still, she definitely felt better taking the supplement cocktail. The speed of her decline slowed, but she was still declining.
She discovered a study using electrical stimulation of muscles in spinal cord injuries. She convinced her physical therapist to add electrical stimulation of her muscles to her physical therapy routine.
Then she discovered the Institute for Functional Medicine and took their course, “A Functional Medicine Approach to Neurodegeneration.” The course talked a lot about the role of mitochondria in neurological disease and the supplements that support mitochondrial function. Her list of supplements grew longer.
Then Wahls had an A-ha! moment.
“What if I took this long list of supplements and said: Where are they in the food supply?” she says. Until then, she had only considered food in terms of which items to avoid; for the first time, she started thinking about what foods to include—and adapted her diet accordingly. “It was the first decision where I said, I’m going to focus on creating health,” she says.
Within a month, her fatigue faded. Her physical therapist saw that she was getting stronger and advanced her exercises. Two months later, at work, she stood up at her desk, walked down the hall, and mailed a letter. Her colleagues were stunned. They hadn’t seen her walking in the hallways in 4 years.
Four months later, she got on her bike for the first time in 6 years and biked around the block. After that, she biked a little every day, gradually increasing the distance. Six months later, she completed the 18.5-mile Courage Ride. “Completing that ride transformed how I thought about disease and health. It transformed my clinical practice and the research that I do,” she says.
Dr. Wahls used what she learned to develop the Wahls Protocol, a guide to using diet to treat MS. Her top recommendations: Cut out sugar and artificial sweeteners and replace grains with vegetables.
Her groundbreaking research and patient advocacy have shifted how researchers think about autoimmune disease and metabolic disorders, how the two are linked, and whether hyperglycemia and insulin resistance trigger the inflammatory response underlying certain autoimmune diseases.
To better understand that question, Dr. Wahls is now leading a new two-year research study, Efficacy of Diet on Quality of Life in Multiple Sclerosis (MS), that will investigate three diets—a modified Palaeolithic diet, a ketogenic diet, and the patient’s usual diet with information provided about the USDA Dietary Guidelines for Americans Diet—for their ability to improve the quality of life and reduce fatigue, which can significantly interfere in the daily life of persons with Relapsing-remitting MS (RRMS). It will also ask whether improving diet can slow brain volume loss. That is particularly important because MS patients have a much more rapid rate of brain volume loss than occurs in those with healthy aging.
What are Autoimmune Diseases?
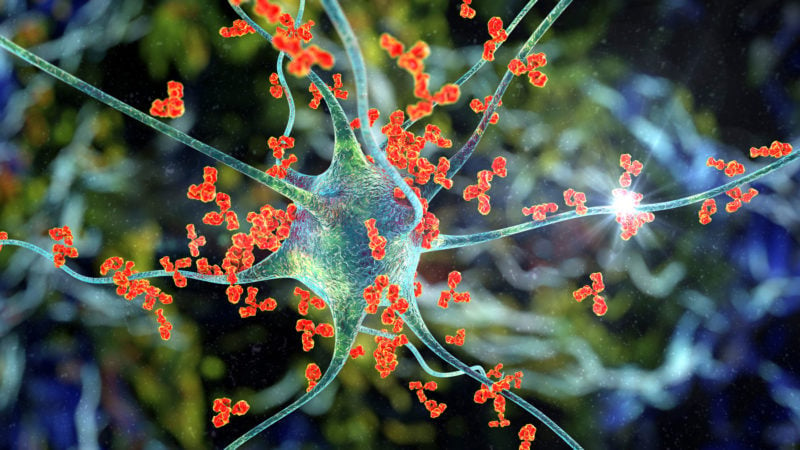
Typically, the immune system protects the body against infection by attacking foreign invaders such as bacteria and viruses. In autoimmune conditions, the immune system mistakenly identifies the body’s own healthy cells as foreign and turns the attack on itself.
More than 80 diseases fall into this category, according to the U.S. National Institutes of Health (NIH), including rheumatoid arthritis, psoriasis, and inflammatory bowel disease. Some autoimmune diseases target a specific organ, such as the pancreas in Type 1 diabetes, while others, like lupus, can affect the whole body.
Autoimmune diseases can be debilitating, especially during flare-ups when tissue attacks are in full swing. Globally, around 4 percent of people live with an autoimmune disease, while in the U.S., up to 8 percent of people are affected. And the prevalence is increasing. Between 1988 and 2012, levels of antinuclear antibodies—blood biomarkers that indicate a person’s chance of developing autoimmune disease—increased from 5% to 13% among U.S. adolescents aged 12-19.
What causes the body to turn on itself is a mystery. “The immune system has evolved to only respond to things that are not part of the body and to dampen the response when it recognizes its own cells,” says Daniel Winer, MD,an associate professor at the Buck Institute for Research on Aging. “That’s called tolerance.”
In autoimmune disease, the immune system loses its ability to tell the difference between its own cells and invaders—a state called “loss of tolerance.” Experts think a genetic predisposition coupled with an environmental trigger such as lifestyle, infection, or exposure likely drives this shift. Some believe the standard Western diet may play a role. Their studies are beginning to establish connections between autoimmune and metabolic diseases driven by elevated glucose and insulin levels.
Research also shows that people with more than one autoimmune disease are more likely to have insulin resistance or Type 2 diabetes than the general population. However, this relationship’s precise nature and direction are not well understood.
“Many diseases that we don’t think have autoimmune components probably do,” says Dr. Winer. “Whether these autoimmune components are merely markers of the disease or they drive the disease is the important question at hand.”
How Inflammation Links Autoimmune Disease and Metabolic Health
Inflammation is a driving factor in autoimmune disease—and it plays a vital role in the onset of insulin resistance and the progression of diabetes, too.
Perhaps most tangible to us as redness or swelling when we cut or injure ourselves, inflammation is our immune system in action. It’s an essential, defensive response to cell damage. But when it persists and becomes chronic, it can cause irreversible damage to tissues and organs.
Here’s a quick primer on how the immune system works. It comprises two arms called the innate (general) and adaptive (specialized) systems. The innate system acts like a first responder. It includes cells such as macrophages (white blood cells that kill microorganisms) and neutrophils (white blood cells that fight infection), which recognize broad structural patterns shared by viruses like the common cold, and, as Dr. Winer puts it, “gobble up anything that looks dangerous.”
Also part of the innate system are tiny proteins called cytokines. These are chemical signals released by our cells. They can be both pro- and anti-inflammatory, and it is only upon their cue that the adaptive immune system kicks in.
The adaptive immune system takes a more targeted tack, using two key cell types: B cells and T cells. T cells are further grouped into two subtypes: CD4+ cells, which orchestrate the adaptive immune response and activate antibody-producing B cells, and CD8+ cells, which sweep in and remove infected cells.
People with autoimmune diseases typically have out-of-balance cytokines. The same is true in insulin resistance. During exercise, however, our muscles release cytokines called myokines, which have a net anti-inflammatory effect. Research has shown that this anti-inflammatory action is the reason that exercise produces improvements in Type 2 diabetes, as well as autoimmune disease.
While the links between hyperglycemia, obesity, and inflammation are well-established, scientists have only recently uncovered details of the process by which excess dietary sugar can cause immune cells to malfunction. A 2022 study showed that GLUT3—a glucose transporter that moves glucose into cells to be converted into energy—also impacts the number of inflammatory cytokines produced by a type of CD4+ T cell called Th17. Since their discovery in 2005, Th17 cells have swiftly become established as significant players in a broad swath of autoimmune diseases.
Researchers are still trying to unpack the complex and multi-layered physiology that drives autoimmune disease. Still, it’s becoming increasingly clear that metabolic disorders and autoimmune diseases share key traits that may stoke one another.
Here’s what we know about a handful of autoimmune conditions that seem to have the strongest links to metabolic health.
Autoimmune Diseases Linked to Metabolic Dysfunction
Rheumatoid arthritis
The link between insulin, glucose and autoimmune disease is arguably most evident in studies of people with rheumatoid arthritis. This painful autoimmune disease causes severe inflammation in the joints and gradually destroys cartilage and bone.
Around 20 percent of people with rheumatoid arthritis also have Type 2 diabetes (compared with about 6 percent of the global population). A large meta-analysis that included more than 1.6 million rheumatoid arthritis sufferers found that, on average, their risk of diabetes was 23 percent higher than normal. Another study from Canada that tracked more than 48,000 people with the disease found that they were 50 percent more likely to develop diabetes over 10 years compared to those with no rheumatic disease.
Inflammatory cytokines play a crucial role in the development of rheumatoid arthritis, particularly IL-6 and TNF-α, which are also seen at elevated levels in people with insulin resistance and Type 2 diabetes. A meta-analysis that pooled data from 14 studies found that in people with rheumatoid arthritis, levels of IL-6 and TNF-α are significantly higher than in healthy controls. Meanwhile, anti-arthritis drugs that target TNF can help improve blood sugar control: A 2019 study found that people taking TNF inhibitors to dampen inflammation in rheumatoid arthritis had significantly reduced risk of diabetes. TNF inhibitors also restore function in β cells (insulin-producing cells in the pancreas), which tend to become impaired as rheumatoid arthritis progresses.
Whether glucose dysregulation is a cause or a consequence of rheumatoid arthritis—or neither—is unclear. Still, it’s well known that steroid medications commonly used to treat the disease can have serious metabolic side effects.
A short, two-week study of men taking potent anti-inflammatory and immunosuppressive steroids called glucocorticoids for rheumatoid arthritis found that the drugs reduce insulin sensitivity in the liver. They also destroy function in pancreatic β cells, which normally act to stabilize rising blood glucose. Because of these effects, people with arthritis who take glucocorticoids for just one month are up to 20 percent more likely to have Type 2 diabetes than those who don’t. After 6 months of medication, users’ diabetes risk jumps by nearly 50 percent, but their risk level returns to normal within three months of stopping medication.
Inflammatory bowel disease
Inflammatory bowel disease (IBD)—an umbrella term for Crohn’s disease and ulcerative colitis—is characterized by chronic inflammation in the digestive tract, which causes pain, ulcers, internal bleeding, and fatigue. Like those with rheumatoid arthritis, people with IBD have an elevated risk of insulin resistance.
Diet has long been implicated as an underlying factor in IBD, but so far, there has been little research in people. Studies in mice, however, offer clues about how glucose impacts the severity of the disease. For instance, when researchers gave mice with ulcerative colitis glucose-rich drinking water, the mice developed more severe colon inflammation than those that drank plain water. The glucose-drinking mice also had higher levels of Th17, the cell type that produces inflammatory cytokines.
Hyperglycemia-induced damage to the lining of the gut could play a role. A 2018 mouse study found that in obese mice, hyperglycemia disrupted the tight junctions between the endothelial cells at the gut-blood barrier, allowing intestinal microbes to escape and spread throughout their bodies. When the researchers looked for evidence of this same effect in people, they found that those with the highest blood glucose levels had the highest number of immune-stimulating microbial molecules in their blood—a situation that likely promotes colitis.
Early research in people has zeroed in on another potential contributor: adropin, a hormone that helps maintain metabolic homeostasis and may play a role in modulating inflammation.
People with IBD tend to have lower levels of adropin than usual. A small study that looked at 30 people with ulcerative colitis and 25 with Crohn’s disease found that both groups had depressed adropin levels—and that those with the lowest levels had the most severe disease symptoms. Other researchers have noted low adropin levels in people with rheumatoid arthritis, cardiovascular disease, and insulin resistance.
Animal studies add to the picture: In mice, adropin deficiency exasperates glucose dysregulation and insulin resistance; a study in rhesus macaques found that animals with low adropin levels have increased risk for Type 2 diabetes—and that fructose accelerates their metabolic dysregulation; and adropin therapy improves insulin resistance and glucose intolerance in obese mice.
Now that researchers have established a link between low adropin levels and IBD, future studies can tease out any causal mechanisms and demonstrate whether a high-glucose diet plays a role.
As in rheumatoid arthritis, however, medications confuse the picture. Glucocorticoids, commonly prescribed when IBD is in a state of a flare-up, nearly triple the risk of Type 2 diabetes in people with IBD according to one extensive analysis—more than in any of the other five autoimmune conditions included in the study.
Lupus
Systemic lupus erythematosus (SLE) is a progressive autoimmune disease that causes inflammation in connective tissues, including cartilage and the lining of the blood vessels. It can damage multiple organs and bodily systems, including the joints, skin, heart, kidneys, lungs, and central nervous system, to a degree that ranges from mild to life-threatening.
So much about SLE remains a mystery, but there is an insulin connection: despite having normal glucose tolerance and pancreatic β cell function, people with lupus have raised fasting insulin levels and lowered insulin sensitivity. They are also nearly twice as likely to have metabolic syndrome compared to healthy controls, according to a large meta-analysis that reviewed data from 24 studies.
A small study in children with juvenile SLE found that they, too, are more insulin resistant than healthy controls—regardless of how long they have been sick or how active their disease is. Crucially, the authors showed that the children’s insulin resistance was not driven by glucocorticoid medicines nor by autoimmune antibodies circulating in their blood.
Doctors aren’t sure exactly how lupus and insulin resistance are related, but studies in adults have turned up clues. A meta-analysis found that people with SLE have elevated levels of a trio of hormones: adiponectin, leptin, and resistin. These hormones are secreted by adipose tissue and play essential roles in regulating insulin sensitivity and inflammation. Strikingly, resistin levels appear to increase in step with SLE disease severity.
In another study, SLE disease damage over time seemed to exacerbate the risk of insulin resistance in people with existing risk factors, including high BMI, large waist circumference, and hypertension—suggesting that insulin resistance is a result, rather than a driver, of SLE.
High doses of glucocorticoids are especially problematic in SLE—upping the risk of insulin resistance more than six-fold. That’s concerning because people with lupus already have a high risk of heart disease, even compared to people with other conditions that raise the risk of cardiovascular complications. A study of primarily females found that people with SLE are 27 percent more likely to have a cardiovascular event––such as a heart attack or stroke––than those with Type 2 diabetes. The authors of that study called for further research to identify the underlying factors that put people with lupus at such a high risk of heart disease.
Multiple sclerosis
Multiple sclerosis (MS) is a debilitating autoimmune disease in which the blood-brain barrier becomes compromised, allowing immune cells to invade the central nervous system. Its core features include widespread inflammation, myelin destruction, neuron loss, and lesions in the brain. There are three types of multiple sclerosis. Relapsing-remitting MS (RRMS), secondary progressive MS (SPMS), and primary progressive MS (PPMS). In 80% of MS diagnoses, the disease follows a relapsing-remitting pattern of active symptoms interspersed with periods of relief. However, with time the vast majority of relapsing-remitting MS will convert to secondary progressive MS and experience relentless decline. Typically this transition to the progressive phase of the disease begins in the late 40s and 50s. In 10% of MS cases, the person has primary progressive MS and never has a relapse, instead having a slow but relentless decline. Around half of all people with MS develop cognitive impairments. In almost all cases, the disease becomes progressively worse with advancing fatigue, mental health problems, and brain fog.
As in other autoimmune diseases, people with MS seem to be at increased risk of metabolic dysregulation. In one small study, people with MS were almost three times as likely as healthy controls to have metabolic syndrome, and nearly half were insulin resistant. Another study found that people with MS were nearly 2.5 times as likely to be insulin resistant compared with controls, even though the two groups’ fasting glucose levels were almost identical and those with MS had overall lower BMI.
How far along a person is in the unfolding of their disease may influence their risk level. A study that looked at 64 people with MS reported that those whose disease was “secondary progressive” (SPMS) were most likely to be insulin resistant. SPMS is essentially stage two of the disease, where disability steadily worsens in people who previously had relapsing-remitting MS (RRMS) for years or decades. In a third category, primary progressive (PPMS), MS is progressive from the get-go, with no periods of remission.
The study found insulin resistance in 74 percent of those with secondary progressive MS, compared with 39 percent of those with either RRMS or PPMS. This effect may be driven by disease duration; participants with SPMS were diagnosed an average of 17 years before the study, whereas those with RRMS and PPMS were diagnosed 9 and 6 years prior, respectively. The researchers ruled out age as a possible confounding factor and noted that insulin resistance was most prevalent among those with the most severe symptoms.
Insulin resistance has also been linked to cognitive dysfunction in MS. A study that looked at 74 people with RRMS found that those with the highest fasting blood glucose levels struggled the most with tasks that required verbal memory, verbal fluency, executive function, and visuospatial processing.
The precise cause of MS remains unknown, but in the last decade, obesity in childhood or early adulthood has emerged as a possible environmental trigger. A study that followed more than 100,000 nurses over four decades found that those who were obese (≥30kg/m2) at age 18 were more than twice as likely to develop MS than those whose BMI was in the healthy range. A Swedish population-based study reported similar findings in people whose BMI was more than 27kg/m2 at age 20.
One leading theory for why this might be the case is that, besides stoking chronic inflammation, obesity disturbs the balance of adiponectin, leptin, and resistin—all of which have been seen in raised concentrations in people with MS.
Skin Conditions
Psoriasis is a common skin condition that often features red and flaky skin and affects around 2–3% of people. But in severe cases, the disease can also increase the risk for cardiovascular events and all-cause mortality. Like other autoimmune conditions, it’s driven by a dysregulated inflammatory response—in this case, in cells that affect the skin, but also have connections to other metabolic conditions, such as insulin response and obesity. This may be why the risk of having metabolic syndrome is twice as high in people with psoriasis compared to people without. The relationship seems to go both ways: One study found that women with psoriasis were 63% more likely to develop Type 2 diabetes, independent of other risk factors, while another study found that as many as 30% of psoriasis cases were attributable to obesity.
Is Type 2 diabetes an autoimmune disease?
Type 1 diabetes and Type 2 diabetes both impair the body’s ability to regulate glucose. Type 1 diabetes is an autoimmune disease—in which the immune system attacks and destroys the insulin-producing β cells of the pancreas, forcing people with the condition to manage their own blood sugar by injecting insulin.
Until recently, Type 2 diabetes was thought of primarily as a metabolic disease—in which factors including obesity and chronically high blood glucose cause the body’s tissues to stop responding to insulin gradually. But over the past decade or so, new evidence has prompted some experts to ask whether Type 2 diabetes should be classed as an autoimmune disease too.
“It’s really in how you define autoimmune disease,” says Dr. Winer. “Do I think there are autoimmune components in Type 2 diabetes? There are. Do I think these autoimmune components are driving the disease? That’s the controversy.”
In 2009 and 2011, Dr. Winer, alongside his brother and their team, published a pair of papers that turned the traditional thinking around Type 2 Diabetes on its head by revealing the role of immune T and B cells in the disease’s pathology.
First, they showed that blocking the action of T cells in obese mice prevented the animals from becoming insulin resistant. Next, they showed that mice engineered to lack B cells were also protected from insulin resistance, even as they grew obese by eating a high-calorie, high-fat diet. They treated another set of obese mice with an antibody called anti-CD20, which helps the body destroy mature B cells. Anti-CD20 is used to treat several autoimmune diseases, including rheumatoid arthritis and MS; in the obese mice, it kept their glucose levels in check. Finally, the researchers showed that overweight people with insulin resistance produce antibodies against some of their own proteins. In contrast, other overweight people do not—suggesting an autoimmunity component to insulin resistance.
“In Type 2 diabetes, there is evidence that the body has lost tolerance to some of the proteins in the pancreas,” says Dr. Winer. Scientists are still exploring whether this is a secondary effect of Type 2 diabetes or whether autoimmunity is a true driver of the disease. Some even suggest that Type 1 and Type 2 exist at opposite ends of a spectrum, where both autoimmunity and insulin resistance are governed by genetics and environmental factors.
One thing is clear: Type 2 diabetes is fuelled by chronic low-grade inflammation, which influences everything from the onset to its unfolding complications. In the years since the Winer brothers published those first papers implicating overactivity of B and T cells, other researchers have added to the picture of the inflammatory landscape in Type 2 diabetes. For example, people with the disease often have inflammation in pancreatic cell groups called islets, characterized by a profusion of inflammatory cytokines, including TNF-α, IL-1β, and IL-12.
Studies also suggest that another class of cells—T regulatory, or Treg, cells—which usually act to suppress inflammation, can’t keep pace with the sheer volume of inflammatory cytokines released by adipose tissue in insulin-resistant people. This sets up a vicious cycle of autoimmunity and metabolic dysregulation: diet-induced inflammation damages tissues, causing them to leak toxins; these cause the immune system to kick into overdrive and attack pancreatic β cells, impairing their ability to secrete insulin and exacerbating hyperglycemia, which drives insulin resistance and more inflammation.
Taken together, these findings are beginning to blur the lines between our traditional understanding of Type 1 and Type 2 diabetes.
Takeaway: Is metabolic health a factor in autoimmune disease?
Undoubtedly, yes.
Poor metabolic health exacerbates autoimmune disease and can accelerate its complications. Adding fuel to the fire, medications commonly prescribed to treat autoimmune diseases are known to induce hyperglycemia and can swiftly increase insulin resistance by an alarming degree. Finally, pain and tissue damage associated with autoimmune disease can make physical activity challenging or impossible, setting the stage for weight gain that may further drive metabolic dysfunction.
Given this confluence of risk factors, people with any kind of autoimmune disease must pay close attention to their body’s ability to control glucose and take steps to curb insulin resistance should it arise.
Many things about autoimmune disease remain unclear, but experts agree that it shares a common inflammatory landscape with insulin resistance and Type 2 Diabetes.
And while myriad things can trigger a state of chronic inflammation in the body—for instance, infections such as COVID-19—plenty of risk factors are within our control, including sleep, exercise, nutrition, and building strong glucose control. By being mindful of these factors, we can give ourselves the best chance of avoiding the chronic inflammation that underpins and exacerbates both Type 2 diabetes and autoimmune disease.