The grim truth about the status of metabolic health in the US is that we are not faring well: 122 million Americans are diabetic or prediabetic, over 70% of the country is overweight or obese, and only 12% of US adults meet the criteria for “metabolically healthy.” Something is clearly not working, and no amount of public health expenditures, blanket dietary and exercise recommendations, doctor’s visits, or pills seems to be getting us out of this public health crisis. Where do we begin in trying to address a monumental issue like this? Todd Rose believes we’d be wise to start by looking at how we collect and analyze health data and that with a bit of modernization in our research practices, the answer might be lying in plain sight.

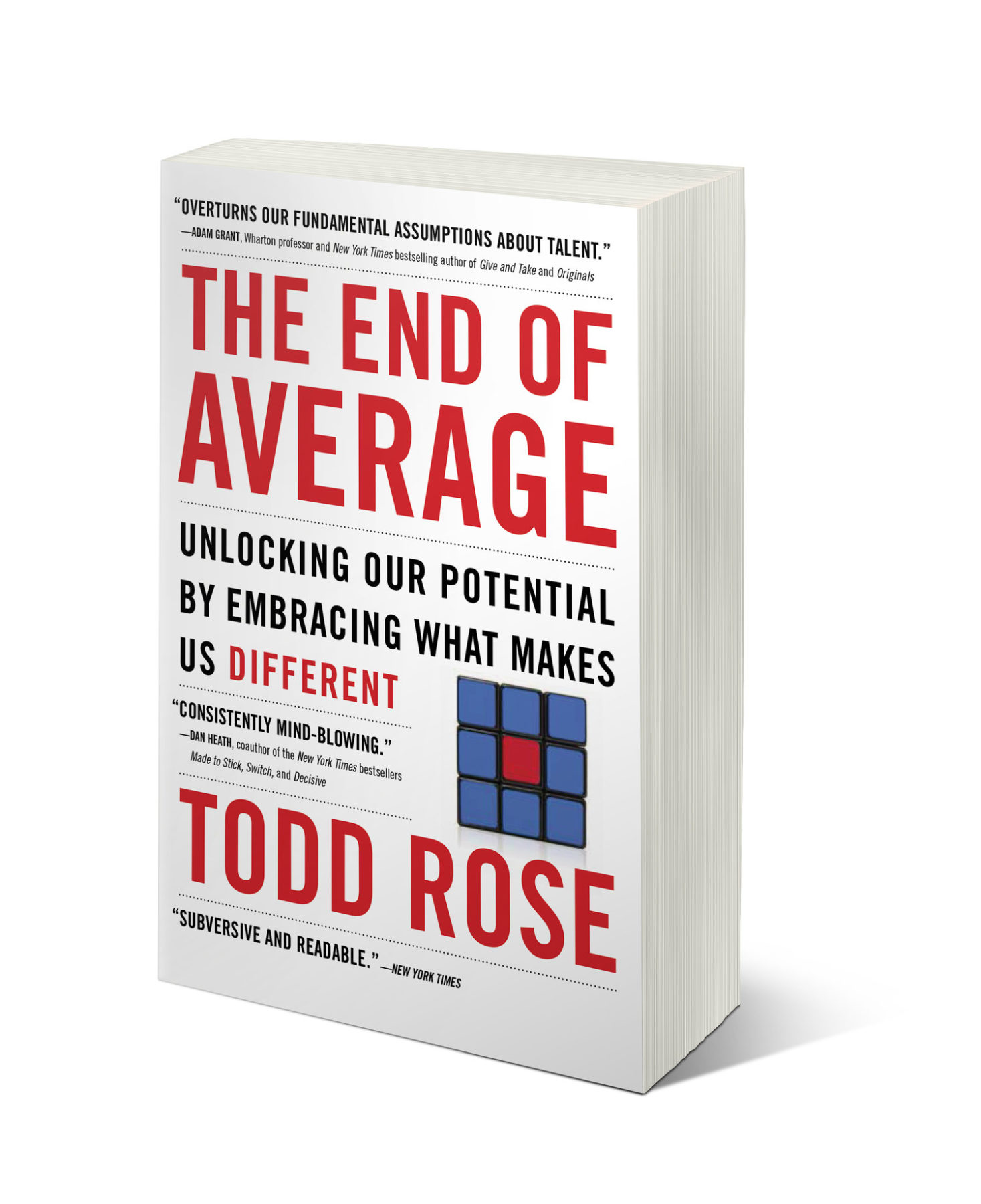
Todd Rose
Rose is the Co-Founder and President of Populace, a think tank dedicated to a new science of individuality, reorienting away from the standard use of averages and aggregates in fields like medicine and education. He’s also a faculty member at the Harvard Graduate School of Education.
Rose has thought a lot about data, and in particular, the implications of the pervasive use of means and averages in biomedical research. His book, The End of Average, argues that too many of our systems—including healthcare—are currently designed for the “average” human and lose sight of the biochemical individuality inherent to human health. Instead, Rose advocates for leveraging new technologies that allow for data centered around human individuality in an effort to move away from cookie-cutter approaches to societal challenges and opportunities.
Levels co-founders Josh Clemente and Dr. Casey Means sat down with Rose to talk about how his research could apply to the metabolic disease epidemic and how individualized data might help improve metabolic fitness on a large scale and empower us to be healthier, happier, and more in control of health.
Why Use Averages?
“Any doctor will tell you that they’ve never seen an ‘average’ patient,” says Rose. “Humans are just too diverse, too unique, to fit a single profile.” That being said, averages can play an important role. It makes intuitive sense that we should prioritize interventions and resources that affect the largest number of people. If we consider a population on a bell curve, this would be those in the largest, middle chunk.
But things get more complicated when we think about humans as complex systems. Categorizing an individual using just one characteristic is untenable; that individual may be smack in the middle of the bell curve for one trait but on the extremes for another. Virtually no person will be “average” for all potential characteristics, so by designing an intervention or program for the “average” person, you may be effectively designing for no one.
Think of pharmaceuticals, for which research has traditionally been based on averages: “If you look at the top-selling drugs in the country and their efficacy rate, it is kind of shocking how small of a percentage of the target population those drugs actually work for,” says Rose. A study may show a positive effect for some chunk of studied individuals, but for a given individual, it may be an abject failure.
Without individualized data, though, this might be our best option. Because we simply can’t consider the individual response of every patient for all relevant outcome metrics, we may need to assume that if an intervention works on average for a group of people for a defined set of metrics, there’s a likely chance that it will work for one specific person.
“Rather than gradually addressing the problem, we only start acting after the catastrophe has happened. Categorical labels like prediabetic or diabetic, are actually masking the real issue.”
Unfortunately, this concept hasn’t held up in practice. When we look at the 10 highest-grossing drugs in the US, we find that for every one person they do help, many others fail to see improvement. On the low end of this spectrum, for every patient who benefits from the arthritis medication Humira, three others see no significant change in their condition. Nexium, the heartburn medication, fares much worse; for every one patient who benefits, 24 do not.
Fortunately, technology is beginning to allow improved individualized applications of data, and researchers like Rose and companies like Levels aim to leverage these technologies to improve health outcomes. Levels does this by facilitating access to real-time, actionable glucose data for individuals via continuous glucose monitors (CGM), allowing people to track their own responses to all dietary and lifestyle choices to improve metabolic health. Gone are the days of needing to have blind faith in a “glycemic index” food chart or a recommended dietary strategy; people can now continuously see the cause-and-effect relationship between choices and their own physiologic response to them.
Issues with Averages
The problems with relying on averages in healthcare don’t stop there. Consider blood sugar measurements. Currently, we use thresholds to decide when an individual should start paying attention to these measurements, based on a number generated by tools like an HbA1c test, among others. Based on these results, an individual is assigned a category: “normal,” “prediabetic,” or “diabetic.”
“The End of Average,” by Todd Rose
The potential harm comes if we ignore blood sugar until it hits a particular “category threshold” number. By the time this number has been hit, the disease state is more difficult to treat or reverse. It’s a bit like digging the well only once you are thirsty. This is especially disconcerting for a disease like Type 2 diabetes, for which the vast majority of cases may be preventable with early attention to diet and lifestyle. “It’s really cold comfort to hear, ‘Well, actually it turns out you were at risk well before, but we’re not even going to bother to think about you until you hit some milestone,’” says Rose.
“Rather than gradually addressing the problem, we only start acting after the catastrophe has happened… [the problem with] these categorical things like prediabetic, diabetic, is that it is actually masking the real issue.” The result is that people march along a spectrum of escalating blood sugar dysfunction well before they meet diagnostic thresholds.
“There’s a little bit of dishonesty involved in thresholds that aren’t really thresholds,” says Rose. “The truth is, from a metabolic health standpoint and fitness standpoint, it is not the case that there is some step change.” Now, with access to CGM data, we have the ability to view personal glucose trends over time, be alerted to patterns that may be early harbingers of metabolic dysfunction, and make informed changes a whole lot earlier.
Averages also make it easy to assume there’s a single path to a problem. When it comes to metabolic dysfunction, if we assume a specific chain of behaviors and biological factors leads to diabetes for all patients, we may focus all our resources on addressing that chain. But Rose notes, “In any complex system, it’s guaranteed that there’s never just one pathway to an outcome.”
Metabolic function is different for every individual, and they may be helped (or harmed) by a completely different course of action than the one we assume is best for the “average” patient. The harm comes when we dismiss a diverse set of routes in favor of a single average route that won’t work for many people.
How Personalized Data—Like That Offered by Levels—Can Change the Game
While averages may always play a role, the rise of new technologies like Levels may make us less reliant on them. By analyzing data on the individual level, rather than on the population scale, we can create a more refined “picture” of an individual’s health over a wide variety of potentially interdependent metrics and more precisely understand the personal impact of lifestyle decisions.
Testing and Refining
Rose doesn’t argue for a wholesale rejection of the averages we use now. Instead, he wants to test them empirically, checking these numbers against a much bigger, higher-resolution pool of individual data. “It’s entirely possible that some of the average-based standards will still hold,” says Rose, “You just have no justification for assuming that they will. You’re flying blind.”
It’s somewhat ironic that the rise of personal data might improve the quality of average standards. “The holy grail is a standard that’s merged authentically out of data on individuals,” says Rose.
Creating a New Context for Health
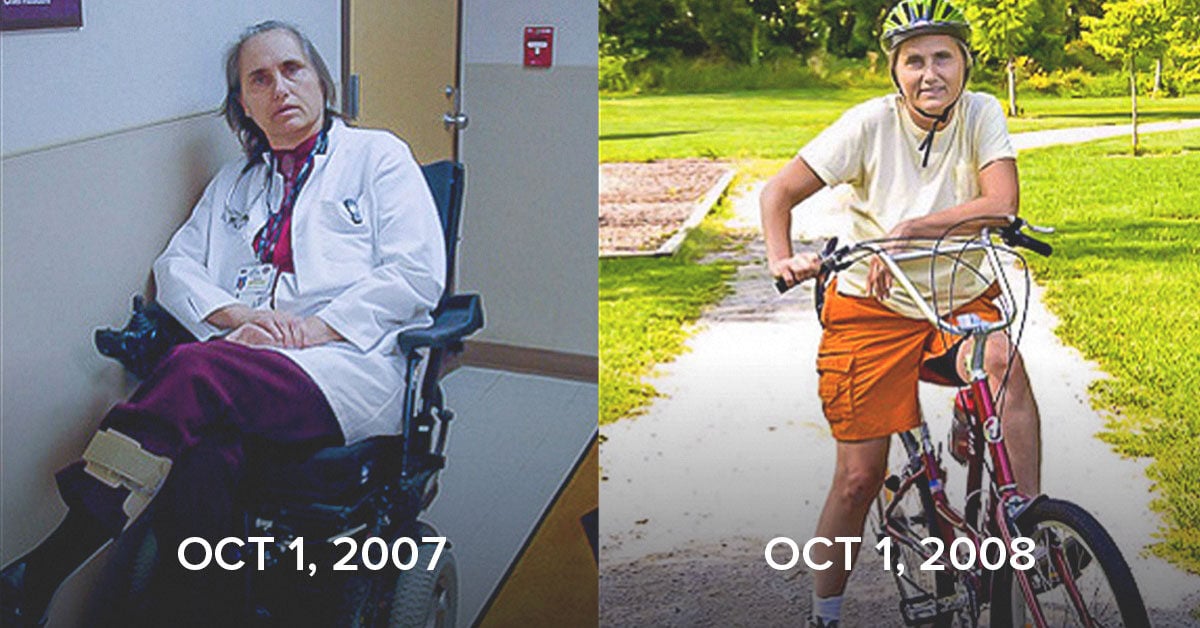
The rise of individualized measurements may also lead to an entirely new framework for thinking about the onset of certain diseases in a way that is extremely empowering. Consider Type 2 diabetes: rather than viewing the onset of disease as a lightning strike that afflicts us at the moment a fasting blood sugar measures 126 mg/dL, we can now observe that disease processes may start years, if not decades, before the moment when someone meets the “threshold” for a disease.
We also know that these biological processes are highly dynamic and can move forward and backward along the spectrum based on diet, lifestyle, and genetics, among many other factors. Individualized data can replace old assumptions with new personalized concepts, allowing for earlier and more targeted interventions.
Individualized measurements may also reveal multiple paths toward a goal. For example, people often use their body weight as a proxy for their overall fitness. Rose himself has done this, and he “forever had thought about weight as the dependent variable.” As he modified his diet, though, he shifted his focus to new data like ketone monitoring that was more actionable for him in reaching his goals.
While this worked for him, the question arises, what might the future look like for society at large? “What we need is a system that allows us to have that high-resolution data on individuals where we can start to build better predictive models of health and wellness,” says Rose.
Conclusion
In short, what your parents told you is true: You really are special. When it comes to overall health and wellness, it’s simply impossible to define your needs based on a single measurement related to a larger population average. Each of us is a highly complex system operating in a unique context, and what may be true for one person isn’t true for another.
Levels is built on the idea that when we have access to our individual metabolic data, we can make decisions that are tailored specifically to our own particular needs. The technology that has made this possible is new, and many of the ideas it challenges are deeply ingrained. We believe, however, that the future of health and wellness is deeply personal, and Levels is built on a simple thesis: the individual matters.