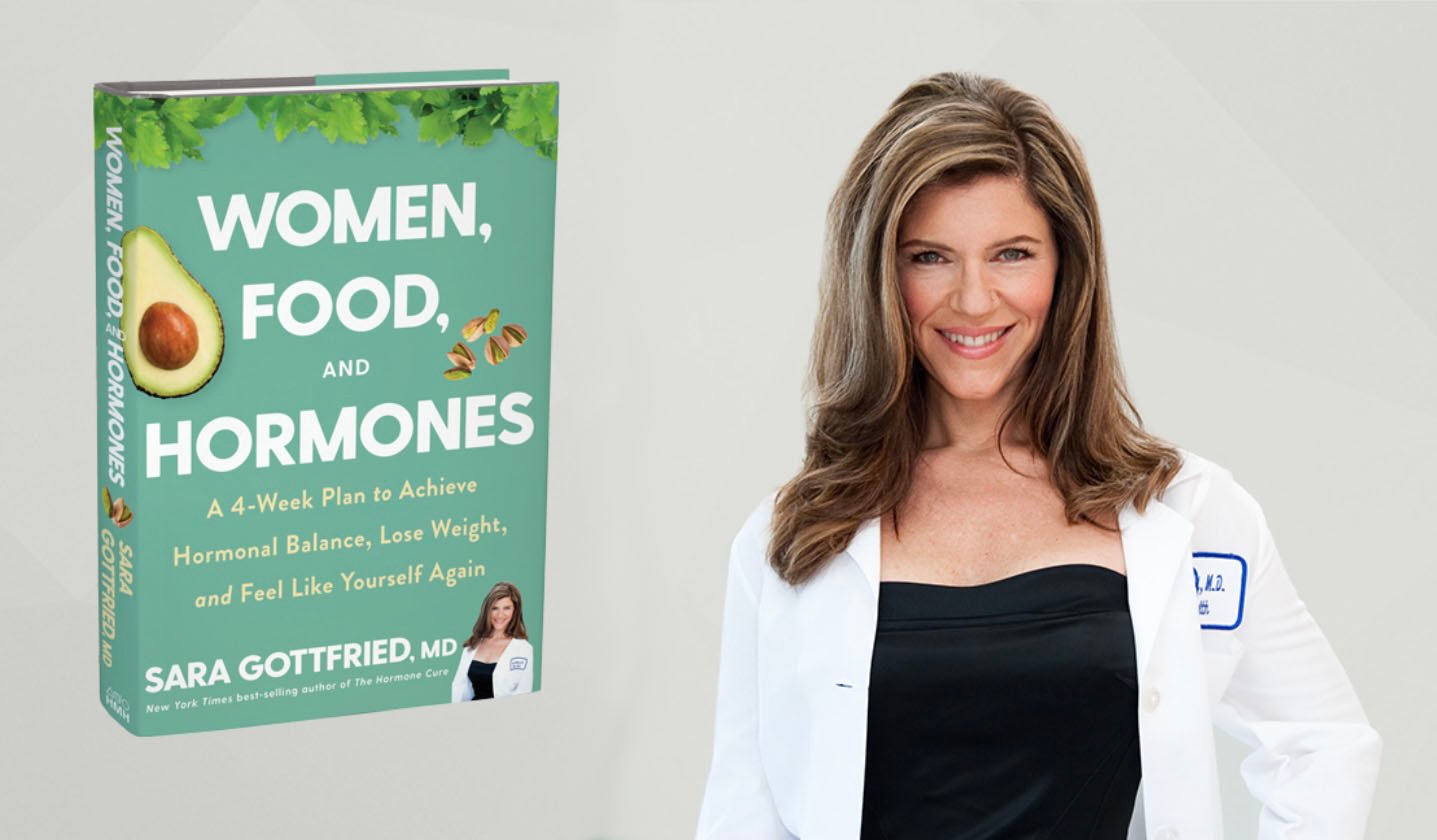
Dr. Casey Means: Dr. Gabrielle Lyon is the queen of muscle, and the creator of the field of Muscle-Centric Medicine. She is also the host of the podcast, The Gabrielle Lyon Show, author of Forever Strong: A New, Science-based Strategy for Aging Well.
Dr. Lyon is a board-certified family-medicine and fellowship-trained physician in nutritional and geriatric sciences. She advocates for the practical application of resistance training for health performance, aging, and disease prevention, and how to use protein effectively to build muscle and be healthy. She is all around one of the most inspiring people I’ve ever met.
Muscle’s Importance Extends Far Beyond Physical Appearance
Dr. Casey Means: Your book has truly changed my life. There are so many people I want to give this to who are feeling stuck in their health journey. I genuinely believe the missing piece is that they’re not focusing on muscle. What’s so cool about muscle is that it’s a whole set of things that you put into your life rather than take out of your life.
You have a very different thesis for what’s going on in our country’s crazy metabolic disease epidemic, and the central thesis of your book is that we are approaching the obesity crisis all wrong. We are focused on fat loss, and we’re not focused on muscle gain and muscle health. Why is this shift important and how can we start bringing a muscle-centric focus into the healthcare system?
Dr. Gabrielle Lyon: I’d love to start with a story about where this came from and how this happened. I did a clinical fellowship in geriatrics and nutritional sciences, and then I did research in obesity medicine at Wash U. We all go into medicine because we want to either alleviate suffering or really make people’s lives better.
At the time, I was working on a study looking at body composition and brain function. I was doing this clinical research, and then my rounds as a physician were in the worlds of geriatric clinics and nursing homes, and centered on the end of life and aging. It was deeply depressing because there’s always a choice as to how we age.
One study participant changed my entire world. Her name was Betsy. She was a mom of three in her mid-50s, with big brown eyes, curly hair, an infectious smile. We all know somebody like that. She had always struggled with weight and obesity—20, 30 pounds, a lifetime of yo-yo dieting, you name it. She cycled through Jenny Craig, Weight Watchers, different kinds of diets, the weight-loss fad. She followed the food pyramid to a T, and the results were devastating. At the end of it all is a really destroyed body composition, meaning a lot of body fat and very little muscle.
At the time, we were doing brain imaging. I imaged her brain and it looked like the beginning of an Alzheimer’s brain. It was at that moment where I knew what was in store for her, and I felt personally responsible. Even though I was not her direct physician, and even though I hadn’t been caring for her for years, I felt responsible. I felt that the medical community had failed her.
The one thing all these people had in common, from the nursing home to the obesity clinic, wasn’t obesity in and of itself. It was the fact that they were all under-muscled. It struck me that for the last 50 years, we were trying to fix the wrong problem. When I asked my colleagues and I looked into the literature, it was still all about obesity.
Again, it wasn’t an obesity problem, which is potentially why we weren’t getting any better at fixing it. It really was having unhealthy skeletal muscle, and that’s where Muscle-Centric Medicine was born. I knew that if I could get this message out to the world, I could change the trajectory of how people age, and that’s what the goal of this book is.
Dr. Casey Means: In my mind’s eye, I can see that patient from my own training: a beautiful, sweet woman or man who has tried to do everything right, and they are going into old age frail, and starting to become decrepit, and have dementia, and it is devastating. We feel hopeless as doctors. We throw up a couple of meds at them knowing exactly what’s going to happen, which is a slow and painful decline toward death, which all of us want to avoid.
I’m going to be totally honest: In my conventional medical training with ENT residency, I never once thought about muscle as a true organ, as a multidimensional organ. I thought about it maybe with sarcopenia patients when the patient was in the hospital bed for five or six days and we’re worried about them losing muscle rapidly, so we give them a bunch of sugar-filled Ensures. That’s basically it.
This is why you’ve blown my mind. Why should people care about muscle and what is your elevator pitch on the suite of things that muscles do?
Dr. Gabrielle Lyon: Let’s start with what people think about muscle. Everybody thinks about the jacked and tan person at the gym. We think about physical performance, but muscle is our metabolic currency. It is our health currency. It is the only actual currency that can’t be bought, sold, bargained for. It has to be earned. And when it relates to metabolism, it is the primary site for glucose uptake.
What is glucose? Glucose comes in the forms of the carbohydrates we eat. About 80% of glucose uptake goes to skeletal muscle. Skeletal muscle makes up 40-some percent of the human body. This is the primary site. When we are talking about metabolic dysregulation, we’re talking about elevated levels of insulin, elevated levels of glucose, elevated levels of triglycerides—all these markers that coalesce into this concept of metabolic syndrome or insulin resistance. A primary focus of this is skeletal muscle.
Skeletal muscle is the metabolic sink, the primary site for glucose disposal, a primary site for fatty-acid oxidation, which is really important to understand. It’s also the primary, and only, site for myokine production. Muscle is an endocrine organ. An endocrine organ secretes these peptides, or myokines, whether it’s interleukin 6 or irisin—there are hundreds of different myokines that are released and that travel throughout the body. This can cause an increase in BDNF, brain-derived neurotrophic factor, for neurogenesis, and helps with overall immune modulation.
Muscle is our metabolic currency. It is our health currency. It is the only actual currency that can’t be bought, sold, bargained for. It has to be earned. And when it relates to metabolism, it is the primary site for glucose uptake.
Myokines can play a role in more than 36 chronic diseases. This is incredible. We can voluntarily control our skeletal muscle. When we contract skeletal muscle, whether it’s through endurance exercise or resistance training, the body releases these myokines.
It’s also important to think about skeletal muscle as an amino-acid reservoir, critical when an individual is in a highly catabolic state, whether it’s cancer or any kind of infection. The body relies on some of these amino acids.
Skeletal muscle is also the body’s armor. If you were to fall, skeletal muscle is where you become mobile. This is tremendous tissue. It probably does more than anything.
Dr. Casey Means: I can’t believe muscle is 40% of our body mass. We just don’t think about it that way. It really comes down to physique, appearance, and strength. That’s what we conventionally think about. But you’re saying it’s actually a hormone-secreting organ. The myokines—again, a word I never heard in medical school—are involved in brain protection and immune modulation.
Having More Muscle Mass Protects Against Inflammation and Disease
Dr. Casey Means: When reading your book, I thought about my training as an ENT. Every single condition we treat is basically an inflammatory condition. You spoke about how muscle is actually an immune-modulating organ. How does muscle relate to our inflammatory chronic-disease epidemic and autoimmune diseases? What does muscle have to do with inflammatory conditions?
Dr. Gabrielle Lyon: I deeply appreciate this question. When we hear about the cytokine storm— and interleukin 6 is considered a cytokine and can cause a cascade of inflammatory reactions, especially if it’s produced from the macrophages, cells of the immune system—that has one effect on the body.
But when interleukin 6 is produced from skeletal muscle, it actually has pleiotropic effects. It can lower inflammation over time. It can also help regulate our metabolism. Exercise helps regulate our metabolism, not just through the increase in mitochondria, but when muscle secretes myokines, specifically interleukin 6, it helps the liver with the metabolism of glucose. It helps the rest of the body with the metabolism of fat. It helps direct the way in which we utilize substrates.
From an anti-inflammatory effect as it relates to autoimmunity, exercise in itself is extremely effective in chronic conditions like rheumatoid arthritis and other rheumatologic diseases. It helps regulate these other cytokines, and that becomes phenomenally important. In fact, exercise is comparable to some medications with its capacity to help regulate and lower immune responses.
Dr. Casey Means: In the book you talk about how having healthier skeletal and more muscle impacts survivability of basically every major chronic disease. We would never conventionally associate muscle with things like heart disease or dementia. How can having more muscle on your body improve our survival from many of these diseases?
Dr. Gabrielle Lyon: Some of this is controversial because we don’t have a great way of measuring skeletal muscle. People often think about DEXA as a way in which we directly measure skeletal muscle. It’s not, quite frankly. A DEXA scan is a way in which we directly measure adipose tissue, and the rest is estimated. Because of this, over time, people don’t relate the amount of skeletal-muscle mass to improvements, which is really important to understand.
People will say strength is more important than mass. I don’t believe that is true. There’s some recent work by Bill Evans coming out with D3-Creatine. We are now starting to be able to measure skeletal-muscle mass directly. It’s currently used in research, but eventually it will get to the general public.
The majority of creatine is in skeletal muscle, so it will allow us to directly measure skeletal muscle versus measuring lean mass. Lean mass is not just skeletal muscle. Lean mass is everything other than adipose tissue. It’s the organs, it’s the bone, it’s everything else. Maybe 40% of lean mass is skeletal muscle. It’s not a direct measure.
Because of that, the amount of skeletal-muscle mass has been largely underplayed. In the literature, people will say that muscle mass doesn’t matter, and that only strength matters. If you were to take a step back, that doesn’t really make sense, because healthy skeletal-muscle mass in and of itself would improve the amount of glycogen storage, which is the storage form of carbohydrates. We know that muscle stores roughly five times more than liver glycogen, because the liver itself is smaller. We have to think about the health of skeletal muscle.
Having more healthy skeletal muscle—in case of an illness, in case of cancer or a highly catabolic process—is going to increase your survivability against nearly all diseases. In fact, the loss of skeletal muscle is likely more critical than the impact of gaining fat.
This is where we move into more healthy skeletal-muscle mass being better. There’s some evidence to support the idea that individuals with obesity carry more muscle, but is that healthy muscle or is that muscle that looks like a marbled steak? Is that skeletal muscle that has fat infiltration?
Athletes also store intramuscular triglycerides as a source of energy. But when an individual is sedentary or struggles with obesity or weight, the fat in and around the skeletal muscle creates issues. It creates low levels of inflammation. There is a decrease in flux. There’s a decrease in substrate fatty-acid utilization. There’s a decrease in glycogen utilization. This stasis, this lack of flux, creates low levels of systemic inflammation, and that becomes a problem.
Healthy and earned skeletal muscle is critical for mitochondrial function, and for generating more mitochondria. You can do this through endurance training. Having more healthy skeletal muscle—in case of an illness, in case of cancer or a highly catabolic process—is going to increase your survivability against nearly all diseases. In fact, the loss of skeletal muscle is likely more critical than the impact of gaining fat.
This changes the paradigm of thinking, because the conversation is all about gaining weight and gaining fat as the issues. Clearly this is a problem, but the loss of healthy skeletal muscle is much more dangerous than the gain of body fat because of the metabolic implications, and because of the survivability going forward. What’s amazing about this story and this paradigm of thinking is that it’s something we actually can do something about.
Shifting Focus: Adding Before Subtracting
Dr. Casey Means: I have the privilege of talking to a lot of Levels members and prospective members. I don’t practice or see patients right now, but I get to talk to so many people who are looking for something to help them feel better. A lot of the people we serve are women ages 35 to 65, and a lot of them are either in their fertility years, perimenopausal, menopausal, or just after menopause.
Some of the things I hear frequently are that they are doing everything right. They feel like they’re eating healthy. They’re buying whole foods. They work out five days a week. They’re managing their stress. And they’re still having trouble—maybe with fertility, or they’re having bad menopausal symptoms, or they’re gaining lots of weight after menopause.
It is heartbreaking, because people are trying so hard. And because of your inspiration, I ask everyone, “Do you resistance train? What are you lifting? What’s your relationship with muscle?” By and large, people haven’t thought that much about it. They’re doing Pilates, cardio—things like that.
For someone trying to lose weight, and for whom robust resistance training is not a part of their paradigm, do you feel that is step one in the weight-loss journey? It’s not about deprivation, but actually what you can build. Should we be reframing wanting to lose 20 pounds, for example, to wanting to build muscle, and the rest is going to take care of itself? Is step building before we lose weight?
Dr. Gabrielle Lyon: Let’s talk about weight loss. We call it weight loss, but what we’re really looking for is fat loss. When we talk about gastric bypass or when people talk about weight loss, what they really want is fat loss.
When you lose weight, typically the maximum amount of fat you could lose per week, depending on how much you have to lose, is two pounds. Anything above and beyond that is typically lean tissue, which is crazy. Dr. Donald Layman did some of the earlier studies, and in people on a calorie-restricted, “Food Guide Pyramid” diet, 30 to 40% of the tissue lost was lean tissue.
We have to think about how we put together a diet and nutrition plan where we’re losing “weight,” but where we’re actually losing fat. For example, if we were to put someone on a 100% starvation diet, which obviously we wouldn’t do, and they lose five to six pounds a week, at least half of that would be lean tissue. This takes us back to the concept of what modalities we are going to use to optimize body composition while losing the appropriate amount of weight. When we think about weight loss just through a calorie deficit, we do nothing about mitochondria function. But if we think about how we lose weight while stimulating skeletal muscle, now we can impact mitochondria.
This is why I focus so much on dietary protein, because everybody is doing it. You cannot get away from eating. If you nail that part appropriately, you have control over your health, wellness, longevity, the way in which you age, and the quality of your weight loss.
We can “lose fat” and do something better, like improve mitochondria function, as opposed to dietary interventions alone. As we have seen with this huge public experiment of yo-yo dieting, people become sarcopenic or suffer from obesogenic sarcopenia, which is the gain of fat and the loss of skeletal muscle. They know what that is, visually, as individuals age—they get skinnier, they get smaller. Sarcopenia is a loss of mass and function, and body composition is the lowest hanging fruit for all health and wellness, and it’s never too late to start, which is incredible to think about.
When we correct for body-composition issues, we optimize for skeletal muscle. The two main ways we optimize for skeletal muscle are focusing on dietary protein and focusing on exercise. I put it in that order because only 24% of the population is meeting the requirements for exercise—resistance training and cardiovascular activity—while 100% of people are eating. This is why I focus so much on dietary protein, because everybody is doing it. You cannot get away from eating. If you nail that part appropriately, you have control over your health, wellness, longevity, the way in which you age, and the quality of your weight loss.
Dr. Casey Means: That makes sense. We’re all eating. And one of the benefits of your approach to diet, which you detail in the book, is that it’s not about deprivation. It’s actually about putting in more of something delicious and starting with adding the protein. It honestly will crowd out other stuff in the diet, and it’s so satiating.
The USDA Food Pyramid doesn’t focus on protein. Many of us don’t even know what it’s like to have a high-protein diet and how it actually can make life easier because we feel more satiated and have stabler energy. It’s exciting because none of it is about starting from a place of wondering what you have to take away.
Why Building and Maintaining Muscle is Essential for Women
Dr. Casey Means: I’d love to talk about women’s health. The female population is being let down by the healthcare system, in terms of really good information for how to age in the most healthy and symptom-free way.
Why is muscle important during the fertility years and going into pregnancy, and around perimenopause and menopause? How can focusing on building more healthy muscle help women in these two phases of life?
Dr. Gabrielle Lyon: Skeletal muscle as it relates to aging is critical for everybody. Pregnancy is an insulin-resistant state. The body has to grow another person within it, and that person needs to get nutrients. One of the major complications with this is gestational diabetes. There are of course genetic components, but there are things people can do to safeguard themselves against gestational diabetes.
I have had two pregnancies. I have a two-year-old and a four-year-old, and one of the things I really thought about and dove into the research on during that time was the impact of skeletal muscle on PCOS, on pregnancy. There’s not actually a ton of information regarding skeletal muscle in pregnancy. If people were to go and look through PubMed or Google Scholar, there’s not a ton there, which is fascinating.
Skeletal muscle, like we talked about before, is the primary site for glucose disposal. Exercise throughout pregnancy is something I personally did, and I did a lot of resistance exercise. When an individual takes in a carbohydrate load and goes for a walk or does some squats or does some pushups, glucose levels will decrease. The reason it’s decreasing at a particular rate, and a rate you can improve upon, is because you’re moving skeletal muscle. Again, the majority of glucose disposal is insulin-mediated. However, you can get away from having to leverage your own body’s insulin when you’re exercising, and this becomes really important for pregnancy.
They say eight to 13% of women will have PCOS. That’s maybe the prevalence; it’s probably much higher. PCOS is polycystic ovarian syndrome, clinically defined as ovulatory dysfunction, maybe androgen excess. It’s estimated that as much as 90% of PCOS individuals will have insulin resistance, and these individuals can be lean or obese. There may be a genetic defect in insulin signaling, but there are probably multiple inputs. Challenges and health issues are not necessarily just one thing. There are typically multiple parts that play a role in a clinical outcome.
However, insulin resistance goes back to skeletal muscle. The primary sites of insulin-targeted tissue are skeletal muscle, adipose tissue, and the liver. The last time I checked, you couldn’t do much about the liver or adipose tissue, but you can do a lot about skeletal muscle.
Dr. Casey Means: What about menopause? I feel this tidal wave of people starting to realize we are so behind on menopause care. Half the population will go through this and doctors have no idea what to tell them. Women go off this metabolic cliff after menopause if they’re not really vigilant about it, because our estrogen drops, and all of a sudden women start outpacing men for obesity and diabetes and Alzheimer’s dementia—two to one with Alzheimer’s.
Every woman I’ve talked to wants to do something about this but isn’t getting complete information. How can muscle impact the menopause journey—the weight gain that might come, and maybe even the menopausal symptoms? Is there any research on that?
Dr. Gabrielle Lyon: Exercise can improve everything. No one has exercised and gone, “Gosh, I From a mood enhancement standpoint, the data support that exercise enhances mood in general, likely because of this influence on BDNF. We also know that the fitter a person is going into menopause, potentially, the lower the significant experience of menopause is. There’s no reason why we wouldn’t try to be the fittest, best version of ourselves going into a potentially challenging time.
That being said, if you are a candidate for hormone replacement, there’s a huge benefit to that. Individuals should not suffer. There’s a lot of good evidence to support estrogen, progesterone, and testosterone. But testosterone, believe it or not, is not FDA-approved for women at this time. There are clear clinical indications that lower testosterone levels in women negatively impact libido and skeletal muscle. These are all really critical reasons why one individual would consider supporting the body’s testosterone.
Going into menopause is the time where I strongly encourage women to reconsider the type of exercise they’re doing. All exercise is good. I firmly believe that Zone 2 cardio is wonderful for people. It helps with endurance, it helps with mitochondrial health—but there are other ways to “skin a cat.” This could be high-intensity interval training. This doesn’t have to be long.
Martin Gibala has done a lot of really good work in this area. I interviewed him on my podcast. There are effective ways to move the needle for people. It doesn’t have to be time-consuming. But if someone is doing exercise, it should be challenging. We have gotten very comfortable. There’s so much stress in other domains of life that, unless you train yourself to actually go in and get after it in the gym, people will typically go there to try to relax or decompress. I strongly suggest women try to do that.
Men and women try to decompress in different ways. When you are going to the gym, three to four times a week of highly focused, intentional training is critical. It should be hard. You should be fatigued. You should go to a point of exertion. You could do high volume and lower weight, or you could do heavier weight and less volume. But overall, and I cover this in my book, women and men should really be thinking about how they are influencing that tissue to get a metabolic adaptation, and there are multiple ways to do that.
Resistance training could be 10 to 20 sets per muscle group per week, and someone could decide on how to do that. Or you could think about getting a well-designed program that could be three to five days a week where you’re hitting each body part twice. Again, there are multiple ways to do it, but what we’re looking for is a stimulus.
Dr. Casey Means: That’s super helpful, practical advice. What about for a woman who exercises five days a week, and is not seeing the results she wants? Maybe there is no strength component to that; it’s mostly cardio, yoga, Pilates, or something else that’s common—a lot of walking, hiking, things like that.
All exercise is good, of course, and we should have a broad range, but do you think most women should be swapping out some of their more cardio-focused or stretching-type exercises for focused, intense resistance training? How would you ideally structure a week for someone?
Dr. Gabrielle Lyon: From a practical standpoint, is what you’re doing getting you the results you want? If it’s not and you don’t have the body composition you desire, perhaps the stimulus has to change. If you have done yoga, Pilates, or walking for years and your body composition has stayed the same, then the metabolic input is not enough for the outcome you are looking for.
We’ve all seen that person at the gym who’s on the treadmill. They’re there six days a week, jogging for 45 minutes, and their body has not changed. If we do the same thing over and over again, as we age, it becomes more detrimental, because now, as hormones shift, the ability to build, protect, and maintain muscle without the proper input decreases.
If we do the same thing over and over again, as we age, it becomes more detrimental, because now, as hormones shift, the ability to build, protect, and maintain muscle without the proper input decreases.
If you are doing your cardio every day and you’re going to the gym, that’s amazing. But what I’d like you to do is swap out three days a week for some kind of resistance training. The literature would say you could do five pounds as long as you’re going to failure. Perhaps you get online, and look for a trainer. We actually have a whole video library we give people, which is amazing.
You have to have a very well-defined and designed program to create stimulus. This is a wonderful time. Be sure not to get injured when stressing the tissue, because what we’re looking for is a metabolic adaptation. We’re looking at stimulus, we’re looking at all the ways in which we can begin to not only increase flex of skeletal muscle, but protect the muscle we have. And if you eat and train the way you did in your twenties, it’s not going to happen.
Why We Need, and How to Get, Enough High-Quality Protein
Dr. Gabrielle Lyon: Over 40% of women over the age of 60 are considered deficient in protein. Without enough protein, we don’t even have a chance of protecting skeletal muscle. Women on average are getting between 60 to 70 grams of protein a day. That’s not enough. If you are going through menopause, perimenopause, postmenopause, this is not enough dietary protein. This is not enough to protect skeletal muscle. When you’re young, this is the prime opportunity to build, but it’s never too late.
However, if you begin to succumb to the challenges of nutrition dogma, which is everywhere, it becomes very confusing. It is not evidence-based. One way to protect skeletal muscle is through increasing dietary protein. You need dietary protein and you need resistance exercise. You need those two things to support health and longevity.
There’s a lot of controversy about reducing dietary protein for longevity, and my answer to that would be, Would you rather be frail and weak and have an extremely poor quality of life, always worried if you are going to fall, break a hip, and not be able to lift your groceries, or would you rather be robust and capable throughout the rest of your life? These are the things we have to be very careful about when we hear this narrative about reducing dietary protein. We’re already not getting enough. We’re not getting enough to support the quality of the tissues we need.
Dr. Casey Means: The book is like the ultimate manifesto on exactly how much protein we need to have and when. People should go to the book for the specific recommendations, but in your newsletter, you’ve focused on a minimum of 30 grams of protein per meal. I love that it’s simple and something you can remember.
Dr. Gabrielle Lyon: That is a very special 30 grams, because people were always asking us about recipes. I know you have Casey’s Kitchen. I have a newsletter that typically talks about the podcast, or some kind of learning resource or study we’re reading. But the 30g’s is a separate newsletter that just provides recipes. I’m hoping you and I are going to collaborate on a recipe.
From a practical aspect, it’s the total dietary protein that matters, but as we age, dosing can impact blood-sugar regulation, mood, energy, skeletal muscle—all of these things. There’s this hierarchy of dietary protein. At the core, we think about how many grams of protein we need per day. At baseline, one gram per pound of body weight is ideal. I’m sure people will read that and go, “That’s so much. I want to be 150 pounds.” That would be a great number to shoot for. You don’t have to have that much. Pregnant women should not go below 100 grams of protein. I do not recommend pregnant women, or anybody, to go below 100 grams of dietary protein a day.
The next thing we need to think about is how we are going to design a plan. The first meal after you are coming out of an overnight fast is, in my opinion, the most important. When you are coming out of an overnight fasted state, skeletal muscle is primed for nutrients. Skeletal muscle is a nutrient-sensing organ. It senses the quality of the nutrition in the diet, specifically the essential amino acids, and even more specifically, the branched-chain amino acids.
I do not recommend pregnant women, or anybody, to go below 100 grams of dietary protein a day.
When you are having a high-quality protein meal—which from a practical aspect would probably be closer to 50 grams of dietary protein—you then push muscle through muscle protein synthesis, which is actually just a biomarker of the meal doing what it’s supposed to do, and you stimulate that tissue in an optimal way. Over time, this protects the skeletal muscle. That first meal is the most important. But that last meal before you’re going into an overnight fast is just as important.
You prioritize dietary protein on the first meal and the last meal, and then for the next macronutrient you can decide whether it’s carbohydrates or fats. I don’t go over a one-to-one ratio of protein to carbohydrates. I cap a non-exercising individual at a maximum of 50 grams of dietary carbohydrates per meal. Again, you have to figure out your carbohydrate tolerance, but there can be a dysregulation of metabolism with too much glucose, and the body can dispose of around 50 grams over two hours in a sedentary individual. For fat, you’ve got to calculate how many calories you need over time, and then you can put fat in there as you wish.
Dr. Casey Means: In the book you talk about leucine as a special amino acid that stimulates muscle protein synthesis on a molecular level and that we need a certain amount of that. Should we be thinking about which foods we’re eating and how much actual leucine is in it?
Dr. Gabrielle Lyon: You actually bring up a very astute point. When have we ever looked at the back of a label—not of a protein shake, but an actual food label—and it says the amino acid breakdown? Never. It doesn’t exist. I encourage everyone to look at the back of a label. It’ll say total calories, total carbohydrates, maybe fiber, fats, monounsaturated fats, whatever else, and then it’ll say protein.
Do you not find that fascinating? We are so behind the times on dietary protein. There are 20 different amino acids that make up protein. There are limiting amino acids. There are nine essential amino acids, which the body must get from the diet. Yet at the end of the day, when you look at the back of a label, it just says protein. These proteins, again, are made up of different amino acids in different ratios. A good rule of thumb is that animal-based products are high-quality proteins. This is not an emotional conversation. This is simply based on the biology and the hard biological numbers of these essential amino acids.
Leucine, isoleucine, and valine are the branched-chain amino acids. You primarily need leucine to stimulate skeletal muscle. It’s a requirement of skeletal muscle, which is, again, a nutrient-sensing organ. Ideally, as you age, you need more leucine because the tissue— through aging, through menopause, through perimenopause—becomes more anabolically resistant, meaning it is less sensitive to the stimulation of dietary protein. This is where that 30 to 50 grams comes from. It’s not just to stimulate muscle protein synthesis, which occurs via the mechanism of mechanistic target of rapamycin, or mTOR. Over time, you begin to lay down tissue.
As we age, this mechanism—this efficiency at sensing protein—lessens. You can overcome this by exercise, increasing capillary blood flow, and dietary protein, in particular the high-quality dietary protein, because it has higher amounts of leucine. That could be through whey protein, that could be through eggs, beef, chicken, fish—whatever it is you enjoy eating. It can also be done through plant-based proteins. But be advised, if you are eating a whole-foods diet, the plant-based proteins often come in a matrix filled with carbohydrates. If you can metabolically tolerate that, then it’s absolutely fine.
Can you get the same stimulus with the plant-based proteins? You can, however, it requires maybe 35% more of total caloric load. For example, six cups of quinoa would equal two and a half grams of leucine. We really have to think about how you can design a diet if you prefer to get your protein from plant-based sources.
Then we have to think about food as a whole-foods matrix. It’s not just about the macronutrient protein. There is creatine, there’s anserine, there’s taurine, there are all kinds of other things that ride alongside high-quality proteins. A perfect diet would be a mix of plant products and animal products, not one or the other.
Dr. Casey Means: If I am thinking about that leucine number, and I’m doing all this strength training, I really want to get the best bang for the buck. I’m putting in the work. How do I actually get the results?
If you’re getting the 30 to 50 grams of high-quality protein in a meal, can you assume you’re getting enough leucine, and enough of the diversity of amino acids?
Dr. Gabrielle Lyon: Yes. There is something called the EAA-9. It’s a proposed new system to look at the quality of protein. It will become very user-friendly, but that is a great way to think about things: if you hit 30 to 50 grams of high-quality protein, you will be getting enough leucine.
The other important aspect of that is that each amino acid has diverse biological roles. For example, leucine is really important to stimulate mTOR. Threonine is important for mucin production, which helps with the gut. There are certain amino acids that are important for neurotransmitter function and glutathione production. There are diverse actions of all these amino acids.
A perfect diet would be a mix of plant products and animal products, not one or the other.
When we target muscle health, the rest falls into place, and that’s what becomes so interesting. If you target skeletal muscle, you’re eating for the health of skeletal muscle, and you’ll hit the other individual nutrient requirements for these other amino acids we don’t even talk about.
Dr. Casey Means: I’m hearing a lot more about creatine. What’s the creatine hot take?
Dr. Gabrielle Lyon: It’s interesting because creatine is stored in skeletal muscle, and women have lower stores of creatine in the body. Creatine is very well-studied. It’s been around for decades. If I were to pick one supplement for a woman who isn’t eating a ton of calories or red meat, creatine would be it. It has an impact on brain function, it has an impact on energy production. Typically, it helps with athletic performance.
There are all kinds of things that creatine has the potential to do. It’s very valuable. There’s even some evidence to suggest that various amounts are needed during different times in a woman’s cycle; she potentially needs more when she’s menstruating. I am not totally convinced on that literature, but over time it’s clear that women definitely benefit from supplementing with three to five grams of creatine a day.
Leveraging Muscle to Stabilize Blood Sugar Throughout the Day
Dr. Casey Means: Something magical about muscle is that it can take up glucose in the absence of insulin. What is happening in the cell to make that happen? How should people be thinking about what to do with their muscles to keep their glucose curves stable?
Dr. Gabrielle Lyon: Let’s start with how glucose is taken up by the cell. This is really a transporter issue, or one of the big ways skeletal muscle takes up glucose. There’s the GLUT4 transporter, which is insulin-sensitive. In the brain, it’s GLUT2, and then there’s also a GLUT1 transporter that is not insulin-sensitive. These are ways in which glucose is removed from the cells, or removed from the bloodstream to move into the cells.
We think about it in a very linear fashion, but in challenges with insulin resistance, there are multiple mechanisms. Is it a glycogen synthase problem? Is it a phosphorylation problem? Is it an insulin receptor problem? There are multiple ways it can impact the system.
This is some of Ralph DeFronzo‘s earlier work. It was really a hallmark when he looked at Type 2 diabetes and insulin resistance and the potential pathways. It’s important to understand that glucose, at high levels, is toxic to the body. A way to move glucose out of the bloodstream and into skeletal muscle is through exercise. This is amazing, this is free, this is something anybody could do. It doesn’t require insulin if you are exercising. Otherwise, skeletal muscle does require insulin.
Again, the GLUT4 transporter is an insulin-sensitive transporter, but through exercising skeletal muscle, you can move glucose into the muscle, which is amazing. That was shown in some of the earlier work from Holloszy, who I had the privilege of meeting at Washington University while he was still alive. He did some of these hallmark studies.
Dr. Casey Means: Is it the muscle contraction itself that’s stimulating some intracellular pathway that’s bringing the GLUT1 or another channel to the membrane? What is the physical stimulus?
Dr. Gabrielle Lyon: The utilization, yes.
Dr. Casey Means: Amazing.
How should someone use muscle throughout the day? Are there any practical strategies for keeping glucose more stable during the day by leveraging muscle?
Dr. Gabrielle Lyon: There are two ways individuals should keep glucose stable during the day. Number one, get your first meal right. It could be a one-to-one ingestion of protein to carbohydrates. When you prioritize dietary protein, the body goes through this process of utilizing protein for gluconeogenesis. Rather than having to eat carbohydrates, your body can make glucose in a way that is steady over time, and that helps with blood sugar regulation. That is just the input of dietary protein with the correction of carbohydrates. It’s super easy. Everybody can do it.
The other thing is to get moving. Again, exercising skeletal muscle will use glucose independent of insulin. If you’re going to have your meal, go for a walk. I know it sounds crazy, but use a treadmill desk. We can take phone calls outside and walk. You also have to know yourself and plan for weaknesses. If you know you are not going to exercise later in the day, plan for that. Suffer a little bit, wake up a little bit earlier, and do it. Again, it’s never too late to start.
Start with three days a week of resistance training. If you do not have time, a high-intensity-interval-training-style workout, if you put enough effort in, could literally be seven minutes. It doesn’t have to be for long periods of time. We’re looking for a physiological adaptation. There are ways in which you can influence the system.
Creating and maintaining healthy skeletal muscle and prioritizing dietary protein will help stabilize blood sugar levels. Unhealthy muscle is like an overstuffed suitcase. No more glucose, no more glycogen can be stored. What happens? You’re going to have increased levels of free fatty acids in the bloodstream because it can’t go anywhere. The muscle is full, the liver is full, the adipose tissue is full. Where is it going to go? It’s going to go back into the bloodstream.
To maintain your health, leverage skeletal muscle, which makes up about 40% of your body composition. Exercising and move that. It doesn’t have to be complex. It just has to be effective.
Dr. Casey Means: I want to talk to you for 10 hours. You are brilliant. Thank God you wrote a book, because you’re scaling your brilliance to so many people. I love how your book heavily focuses on mindset; that’s a very unique aspect.
Dr. Gabrielle Lyon: Thank you. That came from years of seeing patients. I can give you the best book in the world, but if you don’t understand your worthiness to achieve the body you want, or being able to merge your future self with your current self to leverage those decisions and think about what the cost of not doing the thing is, I couldn’t just put a book out there telling you what to do. I needed to be able to take the experience of a physician and what actually makes the art of medicine and leverage that so people can get the best out of themselves.