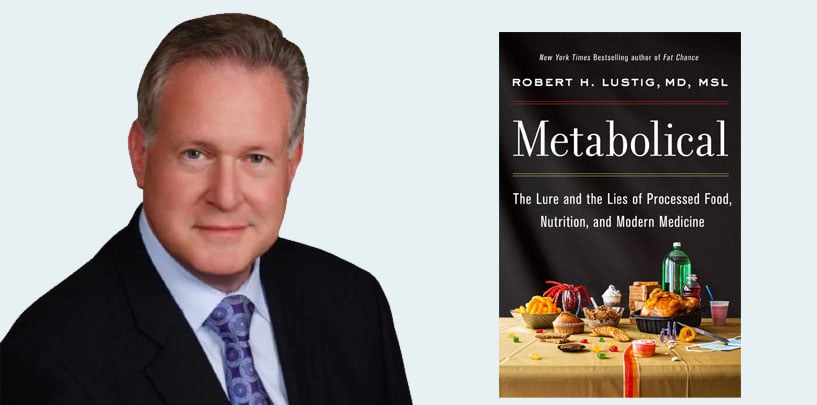
Rob Lustig is a New York Times bestselling author, and one of the world’s leading experts on metabolic health. He’s an emeritus professor of pediatrics at the University of California, San Francisco. Dom D’Agostino is a professor at the University of South Florida, Morsani College of Medicine. He’s also a research scientist at the Institute of Human and Machine Cognition. Both are not only advisors and friends of Levels, but are very much an inspiration to our entire team through their work, their personal lives, and the lifestyle choices they make.
Dom and Rob sat down to discuss insulin resistance. What exactly is insulin and what leads to insulin resistance? What can we do about it? What’s the difference between insulin resistance and Type 2 diabetes? If insulin is so important, why is it not part of regular blood panels and testing?
They provide a better understanding of what exactly it is, how we can think about it, and what to do next.
Insulin, Insulin Resistance, and Why We Should Care
Dominic D’Agostino: I’m excited to cover this topic of insulin resistance—what we know, what we don’t know, what we have to learn, and what actionable things we can do.
Rob Lustig: Indeed. Glad to see you as well. Between the two of us, I think we’ll be able to knock this out of the park.
Dominic D’Agostino: There’s a lot to discuss. It’s central for metabolic health. It’s the etiology of so many of the major chronic diseases, including diabetes, of course, but also all the way to cancer and cardiovascular disease. Let’s talk about what insulin resistance is. How do we define it?
Rob Lustig: Before we define insulin resistance, we ought to define insulin. Insulin is a hormone. It’s a chemical that is made in the pancreas, circulates in the blood, and goes to different parts of the body to do different things in different tissues.
The main thing insulin does is store energy. Insulin is the energy storage hormone. It shunts energy in the form of glucose, and sometimes other foodstuffs—like amino acids and fats—into tissues, especially adipocytes (fat cells) to accumulate energy. Insulin makes fat: more insulin, more fat. The phenomenon of insulin resistance has always been a question mark, because people say, “If it’s more insulin, more fat, if you’re insulin resistant, how come you get even fatter?” This of course is the big paradox in insulin resistance, and we’re going to try to answer that today.
Dominic D’Agostino: A question we get quite often, even from medical students, is, “What is the difference between insulin resistance and Type 2 diabetes, and how do you define it? Does one precede the other?” Insulin is one of the most important metabolic hormones. I don’t think anyone would dispute that.
Another question that comes up in the medical curriculum is, “Why are we not measuring insulin? Why is insulin not part of a comprehensive metabolic panel?” Two questions there. We’d like your insights from a clinician’s perspective.
Rob Lustig: Why is insulin resistance the big issue? The answer to that goes all the way back to 1959, when Rosalyn Yalow and Sol Berson first developed the radioimmunoassay. Their first attempt was to measure insulin. When they took the blood of people with Type 2 diabetes, they expected to see no insulin. After all, they have diabetes.
But what they saw was that the insulin levels were actually higher. They thought, Did we get this right? Are we measuring the right thing? Not only were they measuring the right thing, but they discovered a completely new and important manifestation of chronic disease, the phenomenon of resistance to a hormone.
How come insulin levels are high when insulin function is low? The answer is because the receptors for insulin—the proteins that bind insulin on the cells—have been down-regulated. They are not working as well because there are fewer of them, and the signaling that goes on beyond that receptor is dysfunctional. That is really what insulin resistance is about. Why does that happen? It happens in different tissues and for different reasons. In fact, those different tissues are important in terms of why insulin resistance manifests different diseases.
For instance, Type 2 diabetes is a manifestation of insulin resistance at the level of the liver. Polycystic ovarian syndrome is a manifestation of insulin resistance at the ovary. Cardiovascular disease is a manifestation of insulin resistance at the heart. Alzheimer’s disease, we are learning, is a manifestation of insulin resistance in the brain. This phenomenon of insulin resistance is extraordinarily important for all of these chronic diseases, but it’s region specific. Different tissues manifest insulin resistance at different times, and it is because of that that we end up with these different manifestations.
Dominic D’Agostino: I’m glad you mentioned the brain. A question that I got the other day was, “Can you have Type 2 diabetes without insulin resistance?” I could not answer this unambiguously with a particular reference. I printed out a couple papers, and I didn’t get a chance to read them. From your perspective, can you have Type 2 diabetes without insulin resistance?
Rob Lustig: No. But you can have a disease that masquerades this Type 2 diabetes without insulin resistance. How do you define Type 2 diabetes? Well, anything that’s not Type 1 diabetes.
We know how to define Type 1 diabetes because there are antibodies in the blood. You can have antibodies against the beta cell. You can have antibodies against ICA2, anti-GAD antibodies. There are zinc transcription factors, the nT8 antibodies. All of these demonstrate immunologic destruction of the beta cell. If you have immunologic destruction of the beta cell, you have Type 1 diabetes. If you don’t, then everybody assumes you have Type 2 diabetes.
That is actually incorrect, because there are many different forms of diabetes that are not Type 1. There’s cystic fibrosis-related diabetes, there’s mitochondrial diabetes. There’s a whole host of different diseases, and there are genetic forms of diabetes known as MODYs, mature-onset diabetes of youth. There are 14 of them because there are 14 different genetic defects that will ultimately lead to beta cell dysfunction and lead to hyperglycemia. Those often get looped in with Type 2 diabetes. Patients with MODY account for about 5% of the Type 2’s. Those patients don’t have insulin resistance. You have to know which patient you’re looking at. But if you have true Type 2 diabetes, you have insulin resistance.
Learn More:
The Liver as “Ground Zero” for Insulin Resistance
Dominic D’Agostino: What’s the ideological cause of insulin resistance? Is that also heterogeneous? Gerald Shulman—I’ve read most of his papers and listened to his Banting lecture—has talked a lot about ectopic fat. Dr. Shulman is really focused on the muscle, and fatty acid oxidation impairment of ectopic fat in the muscle, but it also occurs in the liver.
If we want to get an early precursor of insulin resistance, should we be looking at ectopic fat? We should be measuring insulin, but also ectopic fat in the muscle and in the liver. A lot of your emphasis has been on the liver, and I’ve certainly got a much bigger appreciation for the liver as the master regulator, even working in mice and rats.
Rob Lustig: Right. Gerry Shulman is of course the ultimate guru, and I wish he were here to say his piece, but Gerry has undergone an awakening of sorts, and I know why. When he started doing all of his analyses of intracellular fat, intramyocellular lipid, et cetera, he was using a magnet for an MRI that was only 1.5-Tesla. It had to be small, and the only magnet he could use was one that fit around the gastrocnemius muscle in the leg.
He knew a lot about muscle fat. Throughout the early 2000s, he was publishing findings saying that this was a muscle fat issue. He believed it. Then in the late 2000s and 2010s, we had the advent of the 3-Tesla magnet. Now we have a 7-Tesla magnet, and that allows for a much bigger circumference.
We could actually start measuring liver fat. The first paper that came out was from Sam Klein’s group, in 2009. They showed it was actually the degree of liver fat that mattered the most. Gerry Shulman went back to the MRI machine and started looking at livers. He realized the liver was even worse than the muscle. In fact, liver fat actually predicts insulin resistance more than the muscle does.
It is true that muscle insulin resistance contributes to Type 2 diabetes and to overall general ill health. I don’t argue that. But when you actually do the quantitation, the real problem is in the liver. That’s now been documented 50 ways from Sunday. The liver is the big issue.
There are three different insulin resistances. Not one, not two, but three. The first one comes from the general fat, the subcutaneous fat. Normally, subcutaneous fat is protective against metabolic disease. It’s where your body wants to put excess energy. It’s the place where insulin stores the energy. You can gain a certain amount of subcutaneous fat without any cost to the rest of the body. But then a certain point comes where you start forcing more energy into those adipocytes, the fat vacuoles start to grow, the perilipin border that encircles that vacuole starts to break down, and the fat in those vacuoles starts to seep into the cell and kill off the cell. Individual fat necrosis then recruits macrophages to help clean up the grease. Those macrophages then secretes cytokines—TNF-alpha, IL-6, et cetera—which then go, via the systemic circulation, to the liver and activate a NADPH oxidase and ultimately lead to insulin resistance.
Dominic D’Agostino: The fat-induced hypertrophy and stretching of the membrane, and then the rupturing, dysregulation, and inflammation associated with that is the driving factor. As we age, those membranes probably become less viscoelastic. That process is probably augmented by age, too.
Rob Lustig: Exactly. Subcutaneous fat can lead to insulin resistance, but only at a very high level. That’s one of the reasons why we have metabolically healthy obese people: They’re stuffing energy into subcutaneous fat, but they haven’t gotten to the point where those membranes have ruptured. That’s the first way to get insulin resistance.
The second way to get insulin resistance is from stress, having nothing to do with energy and nothing to do with food. The reason we know this is because patients with endogenous clinical depression who are not eating—they’re anhedonic, they are suicidal, you have to admit them to the hospitals to keep them from hurting themselves—are losing weight. They’re losing subcutaneous fat, but they’re gaining visceral fat. You can actually see the visceral fat on the CT scan.
In fact, they have insulin resistance, too. They have it because of cortisol. They have it because of an altered sympathetic nervous system output. They have a different form of insulin resistance, which is not necessarily food driven or energy driven, but rather hormonally driven, like we see in patients with Cushing syndrome.
Then finally, the third group includes the patients with liver fat. Over 45% of the American population and 32% of the world’s population have non-alcoholic fatty liver disease. This is true throughout the entire world. One quarter of all the people on the planet—two billion adults—have fatty liver disease.
Prior to 1980, if you had fatty liver disease, you were an alcoholic. But these are not alcoholics. We don’t have two billion alcoholics. Why do they have liver fat? Why is the liver fat generating insulin resistance?
The liver is the primary target of insulin action. When your liver cells start accumulating fat, they don’t work very well. Your pancreas has to make extra insulin to make the liver do its job. The liver is a really ground zero for why we have this phenomenon of insulin resistance, and that’s why you can be thin and insulin resistant as well as fat and insulin resistant.
What We Eat Matters: How Diet Impacts Insulin, and What We Should Do About It
Dominic D’Agostino: If the muscle has impaired fatty acid oxidation, then could that be the site of impaired glucose oxidation and fatty acid oxidation? And then does that contribute to the buildup of fat in the liver? Or do you think one precedes the other?
I didn’t have an appreciation for the history of the imaging—how the first measurements were made in the gastrocnemius, and then how the 3-Tesla evolved to image the whole body. I’ve always pictured it from the context of impaired fatty acid acid oxidation in the skeletal muscle, which is the glucose sink, and then that creating the bottleneck, which then contributes to the impaired fat oxidation in the liver and de novo fatty acid production in the liver.
Rob Lustig: I believe it can. I’m not saying it can’t. But there’s one piece of scientific evidence that would argue against that, and that is the fat insulin receptor knock-out mouse, the FIRKO mouse. As you know, Ron Kahn’s lab at Joslin Diabetes Center created eight separate tissue-specific insulin receptor knock-outs. They’re all insulin resistant in their own ways, but they’re insulin resistant in different tissues. They have region-specific insulin resistance, and they all have different diseases.
For instance, my favorite mouse of all time is the podIRKO mouse, the glomerular podocyte insulin receptor knockout mouse. This mouse has had its insulin receptor extracted by transgenic means by Cre-Lox from the kidney. The animal is completely, totally insulin sensitive except for in the kidney. This animal has normal blood glucose. This animal has normal ketones. This animal has normal insulin tolerance. This animal is not fat, but this animal has the worst diabetic nephropathy on the planet, even though the animal is euglycemic, even though blood glucose and the glucose tolerance is completely normal.
How can that be? How can you have diabetic nephropathy with normal blood glucose? Because it’s not the glucose, it’s the insulin. The insulin makes the difference. In Gerry Shulman’s research, yes, there is absolutely defective fatty acid oxidation in the muscle. No argument. I agree with that. The question is, is it cause or effect? I believe in most patients, it’s effect, because of the hyperglycemia that’s ultimately leading to it. The reason I feel that way is because of the FIRKO mouse, which is not fat and is not diabetic.
Dominic D’Agostino: If it was in the muscle, then exercise, a very powerful activator of AMPK independent of PI3K, would quickly reverse that, but maybe not so much in the liver.
Dominic D’Agostino: It brings up some questions related to athletes who are consuming 200 to 300 grams of sugar a day but maintain low insulin. But they’re on a different spectrum. We just published a study which found that high-carb athletes are essentially pre-diabetic, even if you adjust for calories, which surprised me.
Rob Lustig: This is the story of Sammy Inkinen, and he’s happy for me to use his name. Sammy is one of the original founders of Nokia. When he was 19 years old, he sold out, cashed in, took his money, moved to the United States, went to Stanford Business School, and started the real estate website, Trulia, which was bought by Zillow for $3 billion. Sammy’s got more money than God.
Sammy was an amateur triathlete, and he would win. This guy exercised five hours a day. At age 38, all of a sudden he realized his performance was going down, and he didn’t understand why. He saw his doctor and the doctor said, “You’re pre-diabetic.”
He didn’t understand: How can somebody who’s a triathlete, who’s exercising five hours a day, be pre-diabetic? He went to see Steve Phinney, who is one of the low-carb physiologists and physicians at UC Davis. Steve Phinney said, “Well, it’s obvious. It’s the sports drinks. Stop drinking the sports drinks.”
Sure enough, Sammy stopped drinking the sports drinks, and his performance went up. His Type 2 diabetes or pre-diabetes reversed. Then what did he do? He started Virta Health. Virta Health now uses the ketogenic diet to reverse Type 2 diabetes, because it knows that even exercise can’t fix this metabolic problem. You cannot outrun a bad diet. You’ve got to fix the diet, first. Yes, exercise is important, but it’s not enough.
Dominic D’Agostino: I connected with Sammy early on, maybe about 10 years ago, when he was transitioning, and met him on occasions. We had a lot of emails back and forth and stuff, too. He really dropped his carb intake. But he would actually add some carbs back in, in the form of 50 to 100 grams of chocolate or dark chocolate—a small amount—when he was doing this crazy rowing feat. It was really interesting.
But then Virta came along. After I met with him at a meeting related to that, I got more and more interested in the use of low carb. I initially thought it was odd to use low-carb diets in athletes because at the time, I was hyper focused on epilepsy because that was the only legitimate application of a ketogenic diet, at least from a randomized controlled trial point of view.
But he opened my eyes about 10 years ago to the application in athletics, as did Jeff Volek and Phinney’s book, The Art and Science of Low Carbohydrate Living. It was really interesting to see that come along. Now the problem exists as a pediatric endocrinologist. It can happen in adults and athletes, but also in the pediatric population, which you were practicing in the ’80s.
Rob Lustig: I graduated med school in ’80.
Dominic D’Agostino: Did fatty liver disease exist in kids in the ’90s?
Rob Lustig: No.
Dominic D’Agostino: Did it start to evolve?
Rob Lustig: I remember my very first case of fatty liver disease. It was in Memphis, Tennessee, and it was 1997. I was called to see this 13-year-old who was pre-diabetic, who was also obese, of course, and who had these enormously high ALT, AST gamma-glutamyl transpeptidases. They wanted to know why he was pre-diabetic. I said, “I don’t know. This is crazy. What’s wrong with this kid?” I figured he had hepatitis C or something like that.
But no, he was negative for all these things. Sure enough, they took him and did a liver ultrasound and saw that he basically had 30% liver fat. I said, “What the hell is this?” That was my very first case of non-alcoholic fatty liver disease. He was only 13 years old, so he wasn’t an alcoholic.
That was my index case. Then they started rolling in after that, and we started looking for it. We realized in 2005 that we could use ALT, alanine aminotransferase, off the chem panel to screen for it. We would also look at fasting insulin in order to determine the degree of insulin resistance. The combination of fasting insulin and ALT was very potent in terms of being able to determine what was really going on with these insulin resistant and fatty liver kids. The answer was two words: soft drinks.
Genetic Abnormalities, and What They Can Teach Us About Insulin Resistance
Dominic D’Agostino: In your practice, did you ever come across kids who have inborn errors of metabolism? I just came from a lysosomal storage disease conference, where we’re doing research on mice who have very large livers. We’re going to do the histology on them, but one thing I didn’t know going into this was that the mice with Pompe disease or glycogen storage disease type 2 have overproduced glycogen and then they can’t break it down.
This causes problems in the muscle, but I was pretty much focused on the muscle and the brain because it’s our wheelhouse. But in communicating with parents who have these kids, the liver is a big problem, and their liver is really swollen and needs to be a focus of attention. But now it’s looked at. Are there genetic predispositions to this?
Rob Lustig: These glycogen storage diseases are actually pretty rare. We have GSD 0, glycogen storage disease type 0, which is glycogen synthase deficiency, all the way up to GSD 9. We have 10 of these diseases. The point is that they store glycogen.
There are certain organs that can store glycogen—for instance, the liver. That’s where your body wants to store glycogen. You can store it in the muscle as long as you can fish it out. Eventually, you can pack enough glycogen in so that it becomes a problem.
But there’s a glycogen storage disease, GSD type 1, also known as Von Gierke’s disease, where you’re missing the glucose 6 phosphatase; you’re missing the ability to get glucose out of glycogen. You’re not able to release it. These patients are enormously hypoglycemic. That’s how they present.
That’s why they call an endocrinologist, because these kids show up with hypoglycemia. They’re in the neonatal or in the early postnatal period and they will stuff glycogen into their livers nonstop. They will be hypoglycemic. They will be ketotic because they can’t use their glycogens. They have to end up using fat, and so they will be ketotic. But the question is, Do they get liver failure? The answer is no. They don’t get liver failure.
Glucose and glycogen are non-toxic. It’s not good to have too much, obviously, but hey, that’s what your liver wants to do with excess energy: make glycogen. That’s why marathoners carb-load before a race. I don’t see glucose and glycogen as being the big problem.
A lot of people think glucotoxicity is the big issue in insulin resistance. There’s some data that supports that. But the reason glucotoxicity is the problem is because, in the liver, glucose is getting turned into fat by this phenomenon called de novo lipogenesis, DNL, where you take glucose, or more likely, fructose, and turn it into fat.
It is the lipotoxicity that actually interferes with liver functioning, not the glucose. It is because of these patients with Von Gierke’s disease that I think so. The glycogen storage diseases play a very minor role in this story. I don’t think it’s as big a problem. The bigger problem is the turning of glucose into fat.
Dominic D’Agostino: In Pompe disease, GSD 2, there’s a hyper source of glycogen and a decrease in autophagy that tends to impair muscle function and becomes painful. That leads to an analogy of what is likely occurring in the liver.
But we probably did not think to look in the liver, and we haven’t really so far. But as we’re starting to do necropsy on these animals, we see that the livers are quite large. The mouse model is new, so we don’t really have a lot of data. But I was thinking it could be somewhat analogous to that.
The Myth of “Calories In, Calories Out”
Dominic D’Agostino: You talked about the fat being the de novo lipogenesis and the accumulation of fat as being the toxin. Would the lipotoxicity be from the swelling? Could it be a mechanical swollen liver that’s breaking membranes and releasing inflammatory factors?
Rob Lustig: I don’t think we know the answer to that yet. What is the fat doing in the liver that’s generating the problem? We know that, for instance, there are pathways that alter insulin receptors.
This is the Hotamışlıgil Harvard School of Public Health story about JNK1, c-Jun N-terminal kinase one: the Syrian phosphorylate is phosphorylating IRS-1 instead of tyrosine. I don’t think we completely know the pathway to a defective insulin receptor yet. We still have to work on that.
Dominic D’Agostino: I understand that Gerald Shulman and other people are looking at ways to augment fatty acid oxidation, perhaps with an uncoupling agent, UCP3, which would be specific to the liver. That would then address the de novo lipogenesis and augment liver fatty acid oxidation.
Do you think that’s a good direction to go into? Obviously we could talk about food—and we’re going to talk about food—but is that a potential strategy?
Rob Lustig: Fixing the liver is paramount. That’s where the action is. Now the question is, Food or drugs? We need both.
Going down Gerry’s route is right, and the reason is because there’s another group that’s also going down that route, and that’s Ron Evans, at Salk Institute. They’ve got a compound that activates PPAR-a, peroxisome proliferator-activated receptor alpha, which is liver specific. This compound is called GW1513. It doesn’t work the same way, but it ultimately does the same thing: It increases fatty acid oxidation in the liver. By doing so, it improves metabolic health. Every which way you turn, the answer comes back to the liver: Fix the liver. That’s one of the reasons I’ve been strongly advocating for, number one, protecting the liver as a primary preventative care measure, and also for treatment for chronic metabolic disease. Of course, that is our entrée into food.
Dominic D’Agostino: In conventional medical education on nutrition and metabolism, we’re taught that there’s not a specific macronutrient, that it’s just an excess amount of calories.
I want you to give an overview, because it would be another three-part series of how, for example, 200 grams of calories from sugar or fructose has a different effect on the liver than, for example, protein or fat. Explain redox control in the liver, and some basic hepatic physiology of handling these things.
Rob Lustig: We’ve been pelted for the last 50 years with calories: Calories in, calories out. Therefore, it’s about two behaviors, gluttony and sloth. If you’re fat, it’s your fault. Therefore, diet and exercise.
Ultimately, all of these are the mantras of the food industry. If it’s about calories, it’s your problem, not theirs. It’s their way of assuaging their culpability for what they are putting into ultra-processed foods. You have to understand that there’s an entire literature that basically pushes back against this notion of calories.
Let me give you some examples. Number one, there are countries with people who are diabetic without being obese, and there are countries with people who are obese without being diabetic. Obesity and diabetes don’t necessarily play the same role.
Number two, obesity is growing at the rate of 2.78% per year worldwide, but diabetes is growing at the rate of 4.07% per year worldwide. If diabetes is just because of obesity, how come diabetes is going up faster?
Number three, if you look at the rate of increase in diabetes in the general population of the United States, it’s going up just as quickly in the obese as it is in the normal weight population. If obesity was the reason, that wouldn’t be the case.
Number four, there are two diseases that we as pediatric endocrinologists take care of that I want to alert you to. One of them is called Laron dwarfism. Laron dwarfism is a defect in growth hormone signaling. There is a founder effect group of Laron dwarfs in Ecuador, and they’re known as the little women of Loja. They were written up in the New England Journal of Medicine. They’re very short, but they’re also very obese. They can’t lift fat out of their fat cells because of the fact that their growth hormone doesn’t work.
These women of Loja should be very sick, shouldn’t they? As it turns out, they get zero diabetes and zero cancer, whereas their wild-type relatives all get diabetes and cancer. They’re fat and they’re healthy, whereas their relatives, who don’t have the growth hormone signaling defect, are all thin and sick. Just being obese doesn’t make you sick.
There is a disease on the other side called lipodystrophy. These people can’t put fat into fat cells because they don’t have it. They don’t have the fat cells to do it, so they end up having to take excess energy and put it into fat in their muscles and in their liver. They have the worst diabetes of all, even though they don’t have any fat stores.
In each of these cases, it’s not about how fat you are. It’s not about calories, it’s not about obesity. The notion that calories are the cause of Type 2 diabetes just has to be stricken. That is not what’s going on. Yes, no question: fat in the wrong places is definitely the problem. Yes, your food contributes to that. But it’s not because of calories per se, because not every calorie is the same.
Dominic D’Agostino: If we’re talking about the general population and you lower the BMI—I don’t like BMI, but, just for simplicity—we can put this into a simple bucket. You treat insulin resistance just by losing weight. You lower your BMI and then you maybe switch to drugs after that to help lose weight.
Rob Lustig: Well, the question is, Where are you losing the weight from?
Dominic D’Agostino: Yes.
Rob Lustig: Are you losing the weight from your subcutaneous fat? Or are you losing the weight from your visceral or liver fat?
Dominic D’Agostino: It’s not going to be one or the other, right? There’s going to be a proportion of each. The faster we can suppress the hormone insulin to augment fatty acid oxidation—which would occur at the level of the muscle, but also at the level of the liver—the better.
On a ketogenic diet, the barometer for enhanced fatty acid oxidation is the production of ketones, because that’s where ketones come from. Ketogenesis is actually driven very site specifically in the liver by accelerated fatty acid oxidation, and that involves carbohydrate restriction. It could occur with calorie restriction; it would be quickly reversed with consumption of sugar. We see that in kids with epilepsy who even get a little sugar from a vitamin. It can kick them out of ketosis and trigger a seizure.
This seems like the low-hanging fruit, if you will. But then there are other drugs like GLP-1 inhibitors and Metformin that people will tinker with before even thinking about dietary intervention, which should really be targeted at lowering insulin, postprandial insulin, spikes in insulin.
How Focusing on the Wrong Things Have Harmed Our Health
Dominic D’Agostino: It leads us back to an early question, which we often talk about in nutrition metabolism class: Why are we not measuring insulin? It was only when I started studying metabolism where I said, “Okay, when I go to Quest, I’ll put the insulin on and start looking at that.”
That’s a problem, because if we see hyperinsulinemia, and we have a Type 2 diabetic who gets diagnosed because their glucose is above 126, could we have caught that half a decade earlier if we were measuring insulin just once or a couple times a year?
Rob Lustig: I couldn’t agree more, Dom. That’s the holy grail right there. Here’s the problem. We have this thing called the American Diabetes Association. I’m not a fan, to say the least. The reason I’m not a fan is twofold. The first is that they state categorically that diabetes is a chronic, degenerative, unremitting metabolic disease with no treatment and no cure. None of those things are true. Virta Health has proven it, among others. You’ve proven it, too. I’ve proven it.
The fact of the matter is that Type 2 diabetes is eminently reversible. You have to fix the diet, but they don’t say anything about the diet. What they said was, “Give all the carbs you want, just give enough insulin to cover it,” which is also not true.
Yes, you can cover the glucose rise with insulin, but all you’re doing is fomenting further chronic metabolic disease. You’re fixing the glucose, but the glucose isn’t the problem. The insulin’s the problem. And the more insulin, the more quickly you die. That’s been shown 50 ways from Sunday, also by a zillion different studies: the United Kingdom Prospective Diabetes Study, the ACCORD Study, the Muraglitazar Study, the ADVANCE Study, et cetera.
The bottom line is, we don’t need more insulin. We need insulin to work better. The American Diabetes Association is basically saying, “Give more insulin,” which is why I am not a fan.
Dominic D’Agostino: You’re saying the American Diabetes Association does not think that insulin is important enough to measure. I think the tide is changing on that. Even my colleague Barbara Hansen, who teaches the med students, has a lot of non-human primate data that clearly shows hyperinsulinemia precedes that.
I’ve never heard anyone put it in those terms. But essentially what they’re saying is that insulin is not important. I’ve heard that there’s maybe not a standardized test for it, and I know it’s tricky to measure, and I’ve used a variety of different approaches, but I don’t know if that factors in, too.
Rob Lustig: That’s exactly right. The American Diabetes Association says, “Do not measure fasting insulin.” I think it’s the most important thing to measure. It’s the first thing I measure, but they say don’t measure it. Why is that?
They say for two reasons. The first reason is, as you just said, insulin assays across the country are not standardized. That is true. One of the reasons it’s not standardized is because certain assays, radioimmunoassays, will pick up other structures that will be confused with insulin, the main one being proinsulin.
Proinsulin is the precursor to insulin. It is a single polypeptide that then has to be cleaved by prohormone convertase 1 in two sites in order to liberate a piece of the peptide called C-peptide. Then you have the mature insulin. When your pancreas is under duress, when it’s trying to lower blood glucose and it can’t because insulin resistance is so severe, it’s got to get every molecule that it’s making out into the periphery as quickly as it can.
That prohormone convertase 1 doesn’t have enough time to cleave off the C-peptide and generate the mature insulin. It will release this immature, non-cleaved form called proinsulin. Proinsulin has about 5% of the activity of the mature insulin molecule. The problem is that proinsulin will get picked up in the insulin assay.
When you measure insulin, especially within a radioimmunoassay, you’re not just measuring insulin, you’re measuring proinsulin, too. Sometimes you’ll even measure IGF-1. Depending on the assay, your assay may not be specific for insulin. That is true. Who cares?
Dominic D’Agostino: Who cares? It’s about relative changes over time, longitudinally.
Rob Lustig: Exactly. The point is, in any given patient, if the insulin’s going up, it’s a problem. If it’s going down, it’s good. That’s all you need to know within any given patient—not how the patient fares against any other patient, but within the same patient. As long as the insulin assay is being done in the same place each time, who cares? That’s problem number one, according to the ADA’s.
Problem number two, according to the ADA: They say fasting insulin does not correlate with obesity. That’s correct. I agree. It correlates with metabolic health for all the reasons we just talked about. Subcutaneous fat is protective. Subcutaneous fat makes up the majority of the BMI. In fact, you can be metabolically healthy, obese, and have low insulin. Fasting insulin does not correlate with obesity. That’s not why you measure it. You measure it to determine metabolic health.
The thing is that fasting insulin will change way before fasting glucose, way before glucose tolerance, and way before hemoglobin a1c. It is a much earlier arbiter of metabolic dysfunction. This is why fasting insulin is part of Levels health’s labs 2.0. The reason it’s there is because I made sure it was. My decision.
Dominic D’Agostino: It’s unfathomable. We are accepting that insulin resistance is a problem and insulin is the most important metabolic hormone. Medical schools know enough about the data to know that insulin starts to go up before Type 2 diabetes is diagnosed. It just seems unfathomable that this is not part of the standard. There’s some historical baggage there with the assays and everything, but geez. What do we do moving forward? Something’s got to change to acknowledge this.
Most importantly, we should probably discuss what is evidence-based. In school, we have to teach about evidence-based therapeutic interventions to treat and reverse conditions. What should be taught from an evidence-based perspective?
Rob Lustig: Having done this for some 40 odd years, we need to get the insulin down any way we can.
The Lower the Better: How to Improve Insulin Levels
Dominic D’Agostino: What are the ideal ranges and what should we do once insulin starts creeping up?
Rob Lustig: Ideally, the fasting insulin should be less than 10 microunits per milliliter. The lower the better. Marathon runners who eat well will have fasting insulins of two or three. I would say anything less than 10 is fine. Once you get above 15, you’ve got insulin resistance, and that’s the breakpoint.
If you have insulin resistance, you are not going to be able to lose weight until that insulin comes down, because that fasting insulin is always there, and it’s always pushing on your fat cell. It’s always telling your fat cell to store more, and you can’t reverse that; you can’t get lipolysis. You can’t get the fat out of that fat cell until that insulin goes down. You’ve got to get insulin down any way you can. There are four ways to do that: diet, exercise, drugs, and surgery.
Diet is where you start. Fix the diet. How do you get insulin down? Very simple. Don’t let it go up. What makes it go up? Really only two things: refined carbohydrates and sugar. Fat does not make insulin go up. Amino acids do make insulin go up, but you need amino acids. Aim for 15% protein—you can go up to 20.
The amino acid that really makes insulin go up is leucine branched-chain amino acids. Branched-chain amino acids are what’s in corn, and corn-fed beef, chicken, and fish. That’s one of the reasons why we also say skip the ultra-processed foods, because that’s basically what corn-fed beef, chicken and fish is.
Dominic D’Agostino: Those foods are high in leucine, and leucine is used as a branched amino acid supplement for many people who lift weights. But you have to view this in context. You’re saying if I do blood work and I measure high levels of leucine, and I don’t work out, that that’s driving insulin resistance? Because the fitness community I’m familiar with is all about, Throw as much leucine as possible in your meals because it’s stimulating muscle protein synthesis. But you’re saying that may not be a good idea? Or in the context of a sedentary person?
Rob Lustig: I was going to say in the context of a sedentary person. If you’re a bodybuilder, you need muscle and you can’t build muscle without leucine. In fact, you can’t build muscle without all three branched-chain amino acids: leucine, isoleucine, and valine. They are 20% of muscle and they are essential amino acids. You can’t make them; you have to eat them.
If the goal is muscle mass, or bulking up, then you have to consume them. That’s why they scoop the protein powder into their smoothies and why they have big tubs of this at GNC. I get it. That’s okay if you’re building muscle.
But what if you’re not building muscle? What if you’re a mere mortal like me and you’re consuming excess branched-chain amino acids? Well, what happens to them? Is there any place to store them? Well, muscle. But if you’re not building it, then you can’t store it there. What happens to the excess? It goes to the liver. The liver takes the amino group off. Now you have a branched-chain organic acid like oxoacetate, which then enters the tricarboxylic acid cycle, and overwhelms the TCA cycle. Vmax, the maximum velocity, can’t turn fast enough, and throws off the excess as citrate. The citrate leaves the mitochondria through a process called the citrate shuttle. Now the citrate is in the cytoplasm. Then those three enzymes—ATP-citrate lyase, Acetyl-CoA carboxylase 1, fatty acid synthase—which we call de novo lipogenesis, new fat making, take that citrate to Asetyl-CoA, then to malonyl-CoA, and finally to fatty Acyl-CoA, which gets packaged.
Now you’ve got triglyceride, and that triglyceride either makes it out of the liver—in which case your serum triglyceride goes up, which is a potential midas for cardiovascular disease or obesity—or it doesn’t make it out and it precipitates in the liver. Now you’ve got a lipid droplet and fatty liver disease. Now you’ve got more insulin resistance.
Dominic D’Agostino: Are you saying this is specific to leucine? Leucine and lysine are purely ketogenic amino acids. Valine and isoleucine are maybe mixed gluconeogenic ketogenic amino acids. Leucine is such a hot topic in the fitness community. The scenario that you described in the liver with leucine—is that specific to leucine?
Rob Lustig: Yeah, that’s specific to leucine, but isoleucine and valine do it, too.
Dominic D’Agostino: Leucine is disproportionately high in certain food products, especially if they’re over consumed and you have excess calories. Then you have a scenario with a surplus of leucine, and with that surplus, the same thing could happen. It’s driving surplus calories in the form of sugar and other detrimental stuff. But it’s that surplus amount of leucine that is really an issue because I haven’t really heard this that much. I remember reading about it in your book.
Rob Lustig: This is work from Christopher Newgard at Duke.
Dominic D’Agostino: Leucine, then, is almost like a biomarker. If you have excess amounts of leucine and you’re not working out, that’s really driving and fueling some of these issues.
Rob Lustig: We don’t tend to draw serum leucine levels, but you could.
Dominic D’Agostino: I just got mine measured. It was in the mid to upper range of normal. But I do eat a lot of eggs and meat and things like that.
Why Fiber and a Healthy Gut Are Essential to Metabolic Health
Dominic D’Agostino: You went through four different scenarios, with diet being the low-hanging fruit. But in your book you also talk about the role of fiber and gut health, the phytonutrients in fiber, how fiber perhaps delays gastric emptying, the mucin layer of the gut. You touch on a lot of different topics, and I encourage anyone who wants a real deep dive and references and everything, check out Metabolical.
Fiber is a contentious topic. I don’t know why it is, but it’s a contentious topic in the nutrition community, especially from the context of a carnivore diet, where fiber is not important or essential. You have people eating zero fiber and claiming that it’s curing their autoimmune diseases and things like that. What’s your take on fiber and why is it important—if it’s important?
Rob Lustig: Your intestine is outside your body. I mean, it’s inside, but functionally, the lumen is outside your body and presents a barrier. It’s a sewer in there, and the goal is to extract the nutrients from what you eat without letting the bacteria or the cytokines or the lipopolysaccharides get across into the bloodstream. If they get across into the bloodstream, they go via the portal vein straight to the liver and induce inflammation. Keeping your intestinal barrier functional and optimal is absolutely essential to metabolic health.
There are three barriers in the intestine. One is physical—that’s the mucin layer. The mucin layer is this mucopolysaccharide coating on top of the intestinal epithelial cells. That basically forms a physical barrier to the sewer. It doesn’t let all the stuff in. The bacteria in the intestine have to live; they have to eat something. They eat what you eat. But the question is, How much did you eat, versus how much did they eat?
If you are absorbing everything early in the duodenum and therefore not presenting anything for them to eat in the jejunum and ilium, then they’re starving. The microbiome and those bacteria get unhappy. If they get unhappy because you’re starving them, they will eat the mucin layer right off your intestinal epithelial cells. They will use it for energy. They will denude your intestinal epithelial cells, and in doing so, they will then increase opposition of bacteria to the intestinal epithelial cell, which you can see on electromicroscopy.
That can ultimately lead to the degradation of that epithelial cell layer and what we call leaky gut. It can also allow bad stuff to get across into the portal system, and therefore into the liver, which can generate systemic inflammation. Fiber is the food for the bacteria. The bacteria will be able to chew it up.
We can’t break the bond of fiber. We can’t break that beta-glucan bond, but the bacteria can. That means that fiber is the food for your microbiome. Increasing the fiber content of food increases microbial diversity. It lets the good bacteria battle off the bad bacteria, which is good from an inflammation and chronic metabolic disease and autoimmune disease standpoint. That’s one reason.
Then there’s the second barrier, which is the biochemical barrier. There are proteins in the intestinal epithelial cells called tight junctions, and they bind cells to each other and don’t let stuff get through the pores. These tight junctions present a complete barrier against the stuff in the sewer, so it doesn’t make it into the bloodstream. Those tight junctions have to work.
The most famous of the tight junction proteins are zonulins, which are the ones that go defective in celiac disease. Well, that’s if they’re immunologically targeted. But you can also nitrate tight junction proteins and they will become dysfunctional and allow stuff to seep through. What nitrates tight junction proteins? Fructose. You increase your gut permeability with sugar. That’s another problem.
Finally, the third part of the barrier is the immunologic barrier. As you probably know, there are more immune cells in your gut than there are immune cells in the rest of your body—all these Peyer’s patches, et cetera. There’s basically an entire immune system running around your intestine trying to keep things out.
Those immune cells, for the most part, are Th17 cells. Those Th17 cells are presenting an immunologic barrier and preventing stuff from getting across as well. But they get depleted on a high-sugar, high-fat diet, and that allows for the entry of stuff you don’t want to get in.
Bottom line: inflammation is in the gut, and the goal is to control the inflammation. There are different things that will control that inflammation. One is getting rid of fructose and controlling those Th17 cells, which of course carnivores do. But fiber is an important one, too. Yes, it’s true. Carnivores don’t do that.
Dominic D’Agostino: Fantastic overview. I need to incorporate some of that into my lectures. But we teach that fiber fuels the production. You touched on short chain fatty acids like butyrate, one of the primary fuels for the colonocytes. Butyrate not only functions as a fuel, but has important signaling properties.
We’re looking at beta hydroxybutyrate. The ambutyrate functions as the histone acetylase inhibitor and has epigenetic function on top of that. It actually helps preserve that brush-border membrane—the barrier function—just by its own anti-inflammatory effects and functioning as a fuel.
It’s interesting that people with Crohn’s disease and other diseases, for example, can be on a diet completely devoid of fiber, and seem to do well on just eating meat. I would not have predicted that. It’s more anecdotal reports and things.
But there’s some research now on the carnivore diet. But any benefit could just be from eliminating things that were toxic or irritating to the gut and triggering a breakdown of zonulin and the tight junctions. It’s not what you’re eating; it’s what you’re not eating that could be causing the therapeutic effects.
Rob Lustig: That’s likely true. Carbohydrates often make the wrong bacteria grow. This may be related to Crohn’s disease. It’s definitely related to autoimmune disease.
This is work from Alan Ebringer, an immunologist from the University of Oxford. He showed years and years ago that patients with ankylosing spondylitis, a classic autoimmune disease, had antibodies against an intestinal bacteria called Klebsiella. It turned out that the Klebsiella was making the enzyme that we use, alpha-1, 6-glucosidase.
Starches are alpha-14 and alpha-16 linkages. If they’re alpha-14 linkages, they’re amylose, which are long linear strings of starch. If they have alpha-14 and alpha-16, then they look more like a tree because of all the branching. That’s why glycemic index is important: it chops up the glucoses off the starch more quickly, because there are more branches, so you can absorb it faster.
It turns out that alpha-16 is not ours; it’s the Klebsiella’s. When you feed starch to a patient with autoimmune disease, they get worse, because you’re actually generating more Klebsiella, and more Klebsiella means more antibody production against it, which then, as an anti-idiotypic antibody, affects the bone and causes the ankylosing spondylitis. This is also true for rheumatoid arthritis, but it’s a different bacteria, Proteus.
What we put in our intestine has enormous ramifications for how well our immune function works based on what we’re doing to our bacteria. This is not a little issue. This is a big issue, and we’ve ignored it in general medicine up to this point. Another reason why we have to watch the refined carbohydrate in sugar.
Dominic D’Agostino: What you’re talking about would also be termed small intestinal bacterial overgrowth from excess carbohydrates. That’s one issue, but I teach that fructose is transported in the gut by the GLUT5. That’s an energy-dependent mechanism.
There’s some evidence that if you load up on a lot of fructose and sugar, it’s not purely diffusion. It’s a facilitated energy-dependent fusion. It could in some ways de-energize the gut. If you consume a lot of fructose, that could cause bloating. Basically, you’re stressing out the intestinal energetic systems by trying to overproduce it.
Rob Lustig: That’s right. You’re depleting the intestine of ATP, and those zonulins are ATP dependent. They’re going to become dysfunctional in the presence of excess sugar. Another reason why sports drinks really don’t make sense.
Dominic D’Agostino: It’s not really discussed how these things, especially fructose, are energy dependent transport processes. If you overwhelm the system, especially in the context of exercising, where you have blood flow diverted from the gut, it can contribute to a lot of performance-related GI disruption and things like that.
A Data-Driven Approach to Fasting, Supplements, and Medication
Dominic D’Agostino: I get this question a lot. It does make sense, from the perspective of eating within a restricted window, to give your gut rest time so it can rejuvenate, make the stem cells, and just sleep. It also ties in with sleep, which is super important. This time-restricted feeding can be used as a way to restore gut health and also to lower insulin as quickly and as much as possible.
Rob Lustig: A paper came out two years ago that suggested that time-restricted eating was very important, but it worked only in those patients with liver fat, and that made sense to me. I haven’t seen a follow-up on that, but that made a lot of sense to me because what that suggested was that time-restricted eating works because it’s giving your liver a chance to get rid of the fat that accumulated over the previous 16 hours, which I think is the right thing to do. I’m for intermittent fasting, but for the right patient. I don’t think it’s for everybody.
Dominic D’Agostino: Makes sense. Another topic I really wanted to cover—because I get a lot of questions about this, and there’s a lot of discussion around it because people want something easy to enhance insulin resistance and facilitate glucose disposal—is the use of supplements.
We know about berberine and alpha-lipoic acid and other things on the market. There’s not a whole lot of evidence behind many of these things, at least for insulin resistance. But in some cases, they may work. What is your opinion and experience with these things? What have you seen in patients?
Rob Lustig: There are a whole bunch of supplements out on the market, and that are advertising on TV. Show me the data, is the way I look at it. They all work in the dish, but I have not seen any of them work in people yet.
Maybe there’ll be a combination that’ll work, but for individual components, there are just no strong pieces of data that demonstrate, in a randomized controlled trial, that any of these have specific and durable effects on fixing insulin resistance.
We have chromium, we have alpha-lipoic acid, berberine, as you said, turmeric, and a whole host of other compounds. But the reason they can put them on the shelf is because they’re supplements. They’re “nutraceuticals.” They don’t have to demonstrate efficacy. I’m a scientist. I’m a clinician. You do have to demonstrate efficacy, and I don’t see it.
Dominic D’Agostino: Good point. There’s a debate with berberine. Some refer to it as the herbal form of Metformin, and maybe there are some small studies out there that compare the two.
I’ve used these things, and I think that, in the context of someone with postprandial glucose excursions, it may knock down the peak of that. But what’s it doing long term, and are there side effects? Also, I don’t think anyone has just measured insulin, which we were talking about. We have a lot to learn before these things can be suggested for patients.
Rob Lustig: I agree.
Dominic D’Agostino: The hot topic now—and we’re talking about it in class—is the implications of these GLP-1 inhibitors.
Rob Lustig: They’re GLP-1 analogues, not inhibitors.
Dominic D’Agostino: Oh, yeah. Analogues.
Rob Lustig: I don’t think we know the answer to that. What we do know is that they cause insulin release. That’s why they work for diabetes. But more importantly, they work at the level of the brainstem to actually tell your brain that you’re full. They’re part of the satiety signal. They always have been. We’ve known that for a long time.
We’re basically telling the brain we’re full all the time, which is one of the reasons these analogues can lead to weight loss: the reduction in food intake. Whether it’s a direct effect on insulin resistance, or an indirect effect because you’re getting rid of the things in the diet that are causing the insulin resistance, is still unknown.
Dominic D’Agostino: It’s a little bit counterintuitive because the GLP analogues do cause a release of insulin and an augmented release of insulin. Are they working centrally and in some way enhancing insulin sensitivity? It’s hard to look at this independent of weight loss, because that’s just a side effect of these drugs, mostly through nausea and things that are unpleasant.
Rob Lustig: Right.
Dominic D’Agostino: To be determined. I guess.
Rob Lustig: At this point, we have the answers for that yet.
Dominic D’Agostino: Thanks for the discussion, Rob. I’ve learned a tremendous amount, and you’ve just further shown that you are an encyclopedia of information on this topic from the clinical perspective, and from the actionable things that people can do.
I commend you for what you’re doing and the information you’re putting out: your books, your podcasts, and everything. You’re helping so many people through the outreach you’re doing, and I really appreciate that.
Rob Lustig: Well, thank you, Dom. You are, shall we say, at the cutting edge of this entire metabolic health movement that is now at the precipice. We are at the tipping point, but I hope that this has been helpful and useful to the general public in terms of understanding why this insulin resistance phenomenon exists, why it’s important, why we as metabolic physiologists focus on trying to understand it and also ameliorate it. This is where the action is.