Metabolic experts and scientists agree that lactate (sometimes incorrectly referred to as lactic acid) is a sorely misunderstood metabolite. This chemical, a metabolic byproduct of glycolysis (or the burning of glucose), spent years relegated to the trash heap of metabolism, thought of as a toxic end-product in oxygen-depleted muscles. In the lab, scientists unfairly blamed lactate for the burning sensations, fatigue, and prolonged soreness associated with exercise. In the clinic, physicians confined it to a narrow scope of applications: testing fitness levels in elite athletes and determining mortality risk in clinically ill patients. High levels in patients with sepsis, shock, or liver failure signal a high possibility of death and placement into a high-risk category in the ICU.
But today, thanks to a growing body of research, this former villain could emerge as a potential hero thanks to a growing body of research. A handful of scientists, led by UC Berkeley biologist George Brooks, have been trying to redefine the role of lactate. They have shown that the body produces the chemical continuously, even in aerobic conditions, where oxygen is plentiful. Its lingering effects do not cause burning, muscle fatigue, or soreness. It turns out that lactate is a potent fuel source for tissues and organs throughout the body. The muscles, heart, and brain utilize the chemical for fuel even when oxygen is plentiful. Some tissues even prefer lactate over glucose when they are injured, hinting at its role as a healing agent.
This evolving understanding of lactate’s role within the body has ignited a paradigm shift. No longer confined to an indicator of exertion or death, lactate is heralded as a potential predictor of disease and, possibly, a therapeutic agent. Scientists are beginning to investigate its potential as a valuable biomarker that offers a glimpse into mitochondrial health and risks of conditions like Type 2 diabetes, obesity, and metabolic syndrome.
What is lactate?
Lactate plays a role in various biological processes. Broadly, it serves three primary roles: to create cellular energy, to help create glucose, and to send signals within the body in response to stressors (like exercise).
Lactate is similar to glucose because it is a building block of cellular energy, called ATP or adenosine triphosphate. Glucose, a sugar, is both ingested in foods and produced in the liver during a process called gluconeogenesis. Lactate is formed during exercise in a specialized type of muscle called “fast twitch” muscle cells. It is produced from glucose during a process called glycolysis in the working muscle and then shuttled into the bloodstream, where it is used as energy by other cells and tissues, such as muscles and the brain. Lactate produced by muscles is taken up in the mitochondria, or “energy factory” of cells, and used to make ATP during respiration. Leftover lactate is transported to the liver and converted back into glucose.
Scientists once thought that cells only produced lactate under anaerobic or low-oxygen conditions. This hypothesis was formed because the early discoverers of lactate, over two centuries ago, found abundant lactate in tissues that lacked oxygen, such as in the muscles of “hunted stags.” These findings and others like them fueled a misconception about lactate. Scientists wrongly assumed low oxygen was a prerequisite for lactate production. This hypothesis came into question around the 1970s, when studies using isotope tracers demonstrated that lactate is produced in the presence of oxygen. Today, there is a growing body of research to back this up, but misconceptions about lactate are still sometimes cited in fitness magazines and the internet.
Lactate is regarded as a major fuel source in addition to glucose. The body maintains a delicate balance between glucose and lactate to meet the energy demands of various tissues, especially during different physiological states such as exercise, fasting, or recovery. Sometimes, organs and tissues prefer lactate over glucose and vice versa. The brain prefers glucose under normal conditions, but in times of stress or when lactate is abundant in the blood (e.g.exercise), the brain and the heart prefer it over glucose. Scientists now know that lactate can provide over 50 percent of the energy needed in working cardiac muscle. And, even in the brain, lactate is a powerful energy source, providing as much as 10 percent of its energy requirements.
In addition, lactate serves a crucial function as a signaling molecule, orchestrating communication among various cells, organs, and tissues. It plays a role in fat breakdown, immune regulation, anti-inflammatory responses, wound healing, and exercise performance, particularly in collaboration with the gut microbiome. Additionally, lactate contributes to gene regulation, immune system activation, and the preservation of homeostasis, which keeps our bodies in balance.
Gradually, scientists are realizing that lactate even plays a role in stress, illness, and injury. After a trauma, such as a head injury, adrenaline activates the sympathetic nervous system, stimulating the production of lactate. Studies in humans and animals with traumatic brain injury have shown it to be a preferred energy source for the brain. There is even evidence that it plays a protective role. In one study, brain-injured rats showed improved cognitive function after receiving intravenous lactate therapy. And even in humans with traumatic brain injury, scientists observed that lactate is the preferred energy source for the injured brain.
Lactate and metabolic health
Lactate is currently being investigated for its potential implications on metabolic health. Studies have linked disturbances in lactate metabolism to conditions such as insulin resistance and Type 2 diabetes. Emerging evidence suggests that lactate may play a role in modulating insulin sensitivity. In one study, lactate levels in fat cells were artificially increased by deleting a gene in mice. As a result, inflammation-causing chemicals called cytokines were released, which recruited macrophages, increased inflammation, and caused insulin resistance in the tissue. These results provide a mechanism for the link between inflammation in fat tissue and systemic insulin resistance in obese people.
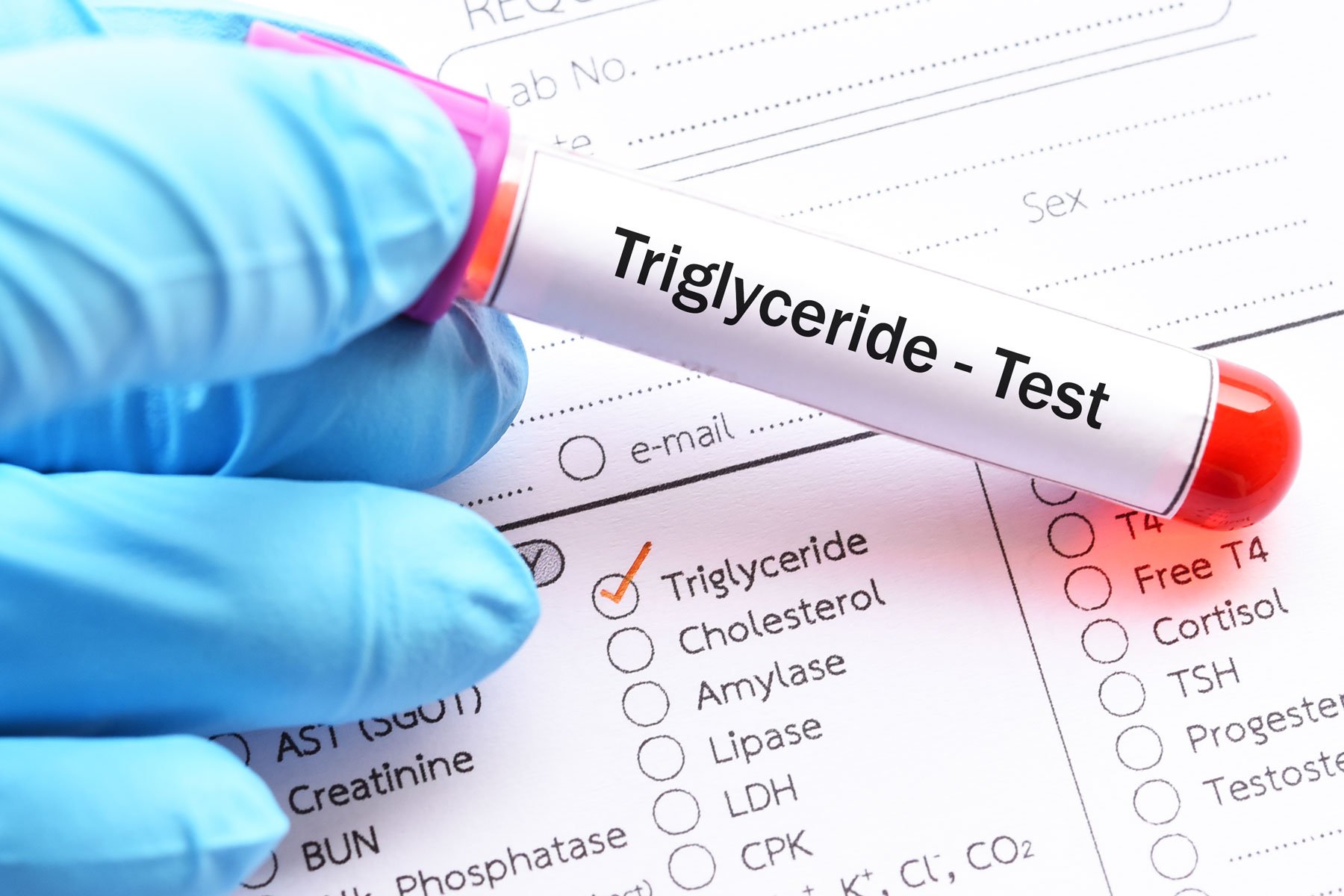
Armed with this knowledge, physicians and scientists are increasingly interested in monitoring blood lactate levels to identify metabolic diseases even before they emerge. A growing body of evidence suggests that lactate may serve as an early warning sign for metabolic conditions such as Type 2 diabetes. For instance, in a study involving older adults (average age was 70), a clear association emerged between blood lactate levels and Type 2 diabetes. Those in the lowest quartile had a 12% chance of having the condition, while people in the highest quartile faced a 30% likelihood.
While this study showed only association, other research hints at a potential cause-and-effect relationship via mitochondrial dysfunction, which is strongly associated with Type 2 diabetes and intracellular lactate concentrations. In a study tracking approximately 8,000 people without diabetes over a 12-year period, a rise in lactate levels—which were used as a proxy for mitochondrial dysfunction—preceded diabetes onset. The study found that blood lactate values above the 50th percentile (≥ 6.3 mg/dL) showed an increasing relationship with diabetes risk.
Some studies have even shown that interventions known to improve metabolic health were associated with reduced fasting plasma lactate levels. One study that tracked elevated lactate levels in obese people showed that the levels came down by as much as 16 percent after six months of endurance training or gastric bypass surgery. In other studies, weight loss showed an effect on lactate. In one, participants who lost five, 11, and 16 percent of their body weight showed corresponding drops in lactate levels. In another study, scientists found fasting lactate levels were higher in participants with obesity, with or without metabolic syndrome, than in lean subjects. When metabolic syndrome patients were placed on a 12 to 20-week low-calorie diet intervention, their lactate levels dropped by 31 percent, with additional improvements in blood pressure, glucose, insulin, and triglycerides levels.
These findings, and others like it, suggest a new role for lactate testing in the clinic. Monitoring levels could serve as an early indicator for identifying people at risk of developing metabolic diseases and as a biomarker for evaluating the effectiveness of interventions.
What impacts lactate levels?
Lactate is constantly produced in the body in muscle cells and then shuttled into organs and tissues, where it fuels energy through mitochondrial respiration. Lactate levels in the body can be raised or lowered by physiological and metabolic factors like exercise, fitness, disease, and genetics. In general, lactate accumulates in the bloodstream when its production exceeds its clearance, like during intense physical activity. In the case of exercise, a person’s specific lactate threshold, or the amount of exercise that boosts blood lactate, can vary based on fitness level. Well-trained athletes may have a higher lactate threshold, meaning they can perform at a higher intensity before experiencing a significant increase in lactate levels.
Other reasons why lactate levels spike involve critical illness. In clinical practice, lactate testing is frequently employed to assess the severity of illness and to measure the response to therapeutic interventions. Conditions like sepsis and septic shock, cardiac arrest, severe lung disease, respiratory failure, pulmonary edema, and trauma can all cause an uptick in lactate. Additionally, seizures, ischemia, burns and smoke inhalation, diabetic ketoacidosis, liver dysfunction, and cancer are culprits.
Some drugs and toxins are also known to boost lactate levels, including metformin, acetaminophen, nucleoside reverse transcriptase inhibitors (NRTI), beta-2 agonists, propofol, epinephrine, theophylline, alcohol, cocaine, carbon monoxide, and cyanide.
Expanding clinical uses of lactate
Accumulating research supports the notion that lactate could be a potential therapeutic in a variety of illnesses in addition to metabolic syndrome.
Cancer
Cancer is linked to abnormal lactate metabolism. Lactate is a potent fuel source for tumors. It can be shuttled to neighboring malignant cells and used as a driver of growth and metastasis. In lactate’s role in cell-to-cell communication, it can promote angiogenesis or blood vessel growth, further fueling the tumor cells.
High lactate production is linked to insulin resistance as well, which is another known factor in cancer progression. Cancer cells can become insulin-resistant, and insulin-resistant cancer patients have a higher recurrence rate. Some research suggests targeting lactate metabolism and shutting it down could be a promising therapeutic for cancer treatment through this mechanism.
Neurodegenerative disease
Studies have shown a link between lactate and neuroprotective factors. One such factor is the Brain-Derived Neurotrophic Factor (BDNF), which bolsters brain health through new brain cell growth and synapse formation. Recent research has shown that increased blood lactate levels (following high-intensity exercise or intravenous infusion) are associated with increased BDNF levels. Other studies linked the increase in lactate and BDNF to improvements in learning and memory. These mechanisms point to a possible therapeutic target for neurodegenerative disease.
The Future of Lactate Research
As scientists unravel the complexities of lactate metabolism, the potential for targeted interventions to improve metabolic health becomes an exciting avenue for exploration. Understanding how lactate influences insulin sensitivity, oxidative stress, overall metabolic function, and more may open new avenues for preventive and therapeutic strategies.
 Learn more about your metabolic health
Learn more about your metabolic health
The best way to understand your metabolic health is with a continuous glucose monitor and an app like Levels to help you interpret the data. Levels members get access to the most advanced CGMs and personalized guidance to build healthy, sustainable habits. Click here to learn more about Levels.

 Learn more about your metabolic health
Learn more about your metabolic health