A continuous glucose monitor (CGM) is a wearable biosensor that can give you real-time information about your blood sugar (glucose) level. This information is vital to people with Type 1 or Type 2 diabetes, for whom high blood sugar levels (hyperglycemia) or low blood sugar levels (hypoglycemia) can be life-threatening. But CGM devices are also valuable for people without metabolic impairment, serving as a window onto how diet and lifestyle decisions affect their health. Consistently high glucose levels or frequent glucose spikes and crashes can lead to short-term health effects like fatigue, brain fog, and depression and are associated with several chronic diseases, including cancer, cognitive decline, stroke, and cardiovascular disease. CGM can help you maintain stable glucose levels before metabolic dysfunction like insulin resistance (prediabetes) sets in and sets the stage for more severe disease.
Here’s a deeper look at this biosensing technology.
What is a Continuous Glucose Monitor?
A continuous glucose monitor is a plastic disc (about the size of two quarters stacked together) that sticks to the skin, typically on the stomach or upper arm. It sends glucose data continuously (at least every 5 minutes) to a smartphone or handheld device, where the user can see it on a graph or chart. People who have Type 1 diabetes sometimes have their CGM connected to an insulin pump that can automatically deliver insulin if their blood sugar gets too high. Most CGMs last anywhere from 7-14 days before they need to be removed and replaced.
There are three primary manufacturers of CGMs in the US: Abbott, which makes the FreeStyle Libre monitor; Dexcom, which makes the Dexcom G6; and Medtronic, which makes the Guardian system.
How Does a Continuous Glucose Monitor Work?
On the underside of the plastic disc is a flexible filament around 5mm long and 0.4mm wide (about as thick as dental floss). When you apply the CGM with the included applicator, a small spring-loaded needle guides this tiny sensor through your skin and retreats (it happens so quickly you typically don’t even feel the needle), leaving the end of the filament in the interstitial fluid just below the skin.
A CGM works by measuring the glucose that continuously seeps from blood vessels and capillaries into this fluid; it doesn’t actually measure blood sugar. The amount of glucose in the interstitial fluid is a close proxy of what’s in the blood, but about 5-15 minutes delayed (the time it takes the glucose to leak into the interstitial space). Many people also calibrate their CGMs with a finger-stick test to improve the device’s accuracy.
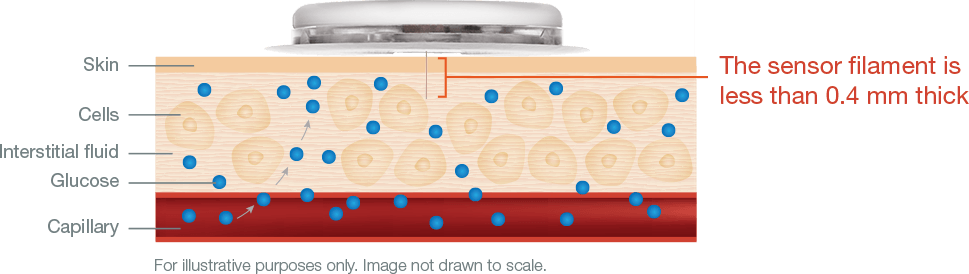
Image courtesy Abbott
Coating the filament is an enzyme called glucose oxidase, which converts glucose to hydrogen peroxide. The hydrogen peroxide reacts with platinum to break down into hydrogen, oxygen, and electrons, which generate current. The device wirelessly transmits this signal to a handheld reader or smartphone, which uses an algorithm to convert the electrical signal to a glucose reading. CGMs have a lifespan of 7-14 days because eventually the chemistry on the sensor degrades, and the reading becomes less accurate.
Future glucose monitoring devices will likely be smaller and last longer, and may measure additional metabolites. They may also incorporate new sensing technology that uses aptamers, or strands of DNA, RNA or amino acids that bind to specific molecules. Aptamers can sense much smaller quantities of a biomarker than current enzymatic sensors.
Learn more:
Why Use a Continuous Glucose Monitor?
One of the benefits of CGM is that it provides a more granular, real-time look at your blood glucose levels than alternative methods such as using a glucometer, which reads glucose from a drop of blood, or glucose tests at your doctor, such as fasting plasma glucose or HbA1c. These other methods provide only a single measurement, a snapshot in time.
This can fail to show you how much your blood sugar is spiking and crashing (known as glycemic variability [more on that below]). They also fail to reveal glucose trends over time or reactions to particular foods. Even if you tested your blood with a blood glucose meter after a meal, you can’t see the entire rise and fall pattern, so your reading may be misleading. A continuous glucose monitor is like listening to the whole symphony instead of just individual notes.
Who Should Use a Continuous Glucose Monitor?
People with Type 1 diabetes can’t make insulin to help maintain stable blood sugar, so they need to monitor their glucose levels closely to prevent dangerously high or low blood glucose. Without a CGM, the only way to do that is to use a finger-prick glucometer dozens of times a day.
But CGMs can also provide several valuable insights that can benefit people with or without diabetes:
- Glycemic variability: This describes the “spikiness” of your glucose curve. Ideally, we want glucose to remain stable and rise only slightly after meals. If you have high glycemic variability, your blood sugar is frequently spiking and crashing. Not only can this impact your mood and energy, but it can also have long-term impacts as well. Studies show that these big spikes and dips in glucose can damage tissues more than elevated but stable glucose levels. Extreme glucose variability has been linked to heart disease, diabetes, and metabolic dysfunction. High levels of variability can also indicate that you’re becoming insulin resistant—your body is unable to use insulin efficiently to control glucose.
- Reaction to individual foods: Our blood-sugar reactions to foods are highly individual. While your blood sugar may spike from a cookie but not from a banana, someone else may have the opposite reaction. Our glucose reactions are also affected by our microbiome, genes, overall fitness, sleep status, stress, and what else we’ve eaten recently. Because of all these factors, simply reading carb content on a label or going by glycemic index is not sufficient to help us find the diet and lifestyle that will allow us to maintain stable glucose. CGM data, on the other hand, provides a far more complete picture.
- Train our bodies to be metabolically flexible: Our body has two primary sources of fuel: glucose and fat. Burning fat produces ketones, which have many health benefits. If our body is burning glucose, it’s not burning fat (in fact, insulin, which is produced when our blood sugar is high, blocks fat burning). Metabolic flexibility refers to how efficiently your body can switch between these fuel sources. Without that flexibility, people may struggle with weight loss, fatigue, or excessive hunger because they cannot efficiently tap into and metabolize their fat stores for energy since their bodies are conditioned to rely on glucose. By using a CGM to help eat for stable blood sugar, we train our body to switch to fat seamlessly when it can.
- Catch metabolic dysfunction early: We can begin to develop insulin resistance more than 10 years before it shows up in our fasting blood sugar test at the doctor. A CGM can help us see our total postprandial blood sugar response, giving us more insight into how our body handles a glucose load. And the earlier we catch metabolic impairment, the easier it is to arrest its development before it reaches prediabetes or diabetes.
Related article:
How Do You Get a Continuous Glucose Monitor?
The FDA has classified CGMs as Class II medical devices, and a healthcare provider must prescribe them. As of 2017, the American Diabetes Association recommends CGMs for people with Type 1 or Type 2 diabetes who need to monitor their blood sugar, although people with Type 1 diabetes still make up the vast majority people who use CGM. Unfortunately, many people with diabetes still struggle to get CGMs approved and covered by their health insurance.
In addition, healthcare professionals are increasingly prescribing CGMs to people without diabetes to help provide them feedback to optimize their health. (So-called “off-label prescriptions” like this make up about 20% of all prescriptions written in the US each year.) In Europe and Canada, CGMs are available over the counter.
Conclusion
Continuous glucose monitoring can improve the quality of life for any individual, whether they have diabetes or not. Access to consistent and accurate data about our blood sugar can help us make informed and healthy diet and lifestyle choices to help support our longevity and wellbeing.











