1. Diet Can Impact Inflammation and Cognitive Health
The Study:
Diet Inflammatory Index and Dementia Incidence
What It Says:
This study, from the National and Kapodistrian University of Athens in Greece, analyzed 1,059 men and women in Greece without dementia and with an average age of 73. The authors looked at the relationship between a diet’s inflammatory potential and the risk for dementia. They used a tool called the diet inflammatory index (DII), which draws food data from 927 peer-reviewed articles that connect different aspects of diet to one or more of six inflammatory biomarkers (IL-1β, IL-4, IL-6, IL-10, TNF-α, and C-reactive protein [CRP]).
“According to the researchers, obtaining and maintaining healthy blood sugar and cholesterol levels starting in younger adulthood can decrease a person’s risk of Alzheimer’s disease several decades later.”
Participants completed detailed dietary food logs and underwent dementia testing for an average of three years. At the end of this time, the researchers calculated the DII scores for each participant. Researchers then divided participants into three groups based on how inflammatory their diet was.
Sixty-two participants developed dementia during the study period, and each additional point on the DII score was associated with a 21% increase in dementia risk. Those in the highest third of DII scores were three times more likely to develop dementia compared to those in the lowest third.
Why It Matters:
To quote the study’s senior author, “Diet is a lifestyle factor you can modify, and it might play a role in combating inflammation, one of the biological pathways contributing to risk for dementia and cognitive impairment later in life.”
In other words, we can control what we eat (and don’t eat) in ways that can influence our brain health – for better or worse.
It’s important to keep in mind that this was an observational study using self-reported food logs. Therefore, it doesn’t prove that an anti-inflammatory diet prevents dementia. Humans are also notorious for inaccurately estimating and tracking their intake.
Nevertheless, various mechanisms are likely at play that associate higher inflammation with poorer neurocognitive health. These include dietary factors such as too much sugar, pesticides, food additives, and other endocrine disruptors. Furthermore, this study joins numerous other studies highlighting the relationship between a healthful diet and decreased risk of cognitive decline.
2. Cholesterol and Blood Sugar Impact Alzheimer’s Risk Later in Life
The Study:
Midlife lipid and glucose levels are associated with Alzheimer’s disease
What It Says:
The study aimed to determine whether a person’s cholesterol and blood sugar levels affect their likelihood of developing dementia later in life. The researchers used data from 4,932 participants of the Framingham Heart Study (FHS). In this study, adults underwent thorough medical, dietary, and lifestyle evaluations every four years for most of their adult lives, giving researchers rich long-term data. For this study, they split participants into three age groups: early (35-50), middle (51-60), and late (61-70).
The researchers found that participants with lower levels of high-density lipoprotein (HDL)—50 mg/dL, on average—had a higher incidence of Alzheimer’s disease (AD)in early and middle age. They also found that fasting blood sugars above 100 mg/dL in the middle age group predicted a higher likelihood of developing AD. Specifically, a 15 mg/dL increase in HDL during early or middle age was associated with a 15% decrease in AD risk; a 15 mg/dL increase in glucose during middle age was associated with a 14.5% increase in AD risk.
According to the researchers, obtaining and maintaining healthy blood sugar and cholesterol levels starting in younger adulthood can decrease a person’s risk of AD several decades later. The researchers also note that these risk factors, especially blood sugar levels, may apply not just to AD but to other types of dementia.
Why It Matters:
Previous studies have supported HDL’s mechanistic role in the development of AD. Since cholesterol levels are modifiable, understanding the precise ways HDL and other lipoproteins impact the buildup of amyloid in the brain can help inform strategies to decrease the incidence of AD. (Amyloid accumulation is thought to be one mechanism of cognitive decline.) Possible interventions could emphasize dietary changes and other lifestyle and medication-focused approaches to optimize cholesterol levels.
Additionally, while the relationship between AD, higher blood sugars, and diabetes has been well established, this is the first study to show that even in people as young as 35 with normal cognition, blood sugar levels impact AD risk later in life for several reasons.
The brain is very sensitive to variations in blood sugar levels. For instance, hyperglycemia can lead to neuron death because it impairs neuron cell functioning. Chronically high blood sugar also leads to high levels of free radicals and cellular stressors. Moreover, high blood sugar can lead to an increased likelihood of cholesterol being deposited in the arteries, especially in the thin arteries of the ventricles of the brain, which are more likely to get obstructed by these plaques. When the arteries are blocked, their brain cells do not receive oxygen or nutrients and die.
In sum, these findings suggest that better HDL cholesterol and blood sugar management beginning in early adulthood could help protect brain health as we age.
3. Younger Age Doesn’t Make the Brain Immune to the Effects of Poor Metabolic Health and Obesity
The Study:
Relations of Metabolic Health and Obesity to Brain Aging in Young to Middle-Aged Adults
What It Says:
This study also analyzed a group from the Framingham Heart Study (FHS)—in this case, people between the ages of 37 and 55 who did not have any diagnosable diabetes, stroke, or neurological disorders. FHS participants had extensive medical testing that included comprehensive lab work and brain MRIs completed every four years, starting in 2002. This study looked at the results of a second exam for a cohort from 2008-2011.
The 2,170 participants were grouped into one of four classifications:
- Metabolically healthy (MH) and not obese
- Metabolically healthy and obese
- Metabolically unhealthy (MU) and not obese
- Metabolically unhealthy and obese
Metabolic unhealthiness was defined as meeting two or more criteria for metabolic syndrome, and obesity was defined as a body mass index, BMI, ≥30 kg/m2 (healthy BMI is considered to be between 18.5 and 25 kg/m2).
Both obese and nonobese MU participants had lower total brain volume compared to the MH nonobese group. It’s worth noting that our brains shrink as we age, so this decrease in brain size for metabolically unhealthy subjects may signify early brain aging.
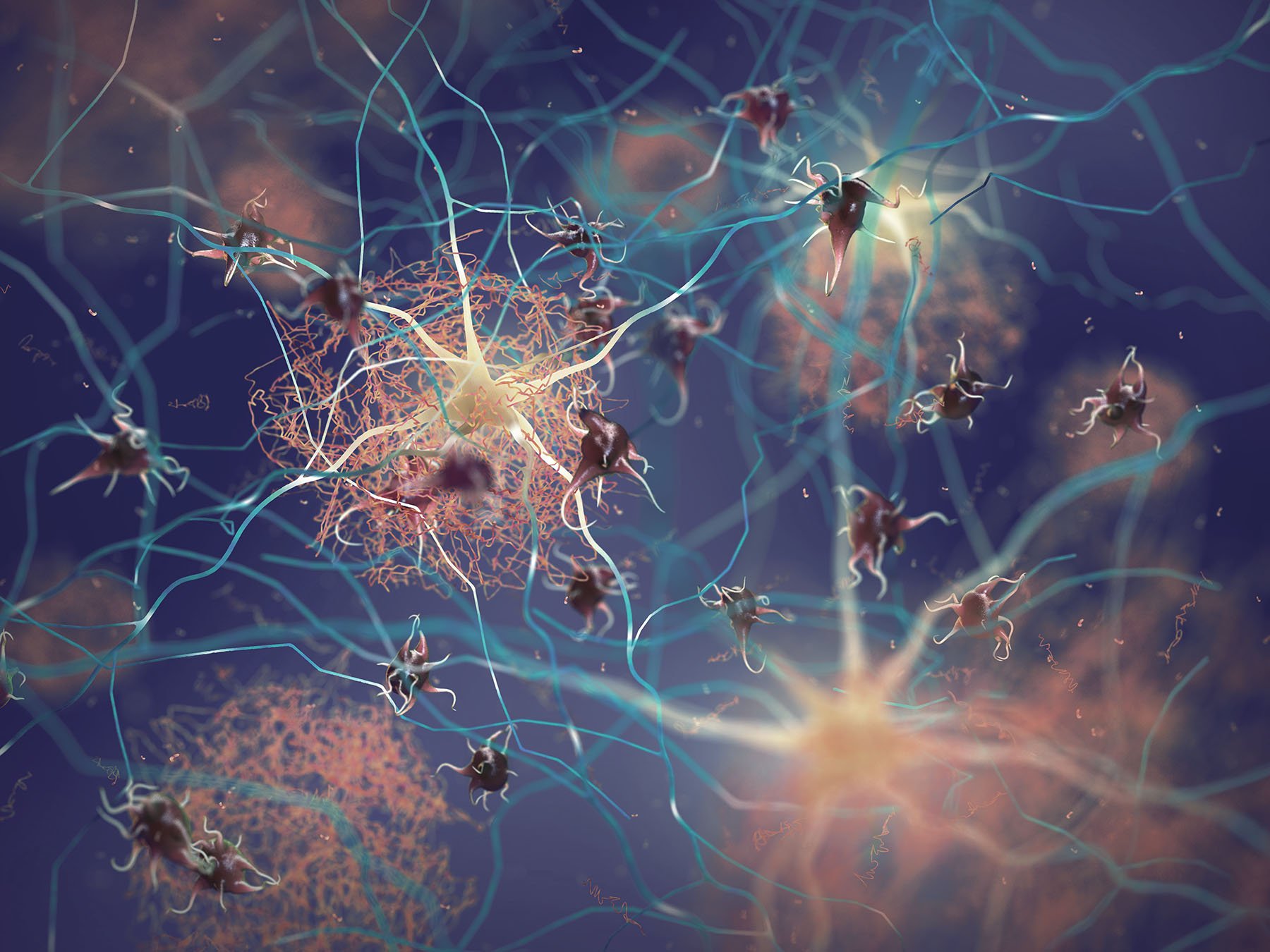
Those who were MU and obese had worse overall neurocognitive scores, including lower levels of global cognition, logic, memory, and the ability to identify similarities and differences between objects. These participants also had more unfavorable brain health markers, including considerably more white matter hyperintensity volume and impaired white matter integrity compared to their MH and nonobese counterparts. White matter is significant because it contains axons that allow neurons to communicate with each other. When white matter is damaged, it impairs high-speed communication between neurons, affecting the brain’s cognitive, motor, and sensory functions.
Why It Matters:
It is important to note that the participants analyzed in this study were White and of Western European origin. This limits the study’s applicability to other racial groups and people of younger and older ages.
Nevertheless, the study does have significant implications.
Most notably, these findings suggest that metabolic dysfunction impacts brain health and that these effects start taking place in relatively younger adults when there is still an opportunity to intervene.
In other words, improving metabolic health and attaining a healthy body mass index may make a difference both in the immediate and long-term—even when overt symptoms are absent.
4. Alzheimer’s trigger may come from areas of the body outside the brain
The Study:
Peripheral Aβ acts as a negative modulator of insulin secretion
What It Says:
Researchers from Osaka City University have found that in mice the brain isn’t the only organ that produces amyloid-β (Aβ). Aβ deposits in the amyloid plaques accumulate in the brains of people with Alzheimer’s disease. They make up the majority of these plaques. This study shows that peripheral organs and tissues sensitive to glucose and insulin—including the pancreas, liver, fat, and muscle—also secrete Aβ.
This animal study demonstrated that these peripheral insulin-sensitive organs also secrete Aβ, and the Aβ modulates insulin secretion—in short, it’s one way the body may “fine-tune” its use of insulin to regulate blood sugar.
Researchers previously believed that Aβ blood levels were indicative of brain pathology alone and have been a diagnostic marker for AD. But this study shows that peripheral tissues also create Aβ through the same amyloid precursor protein (APP)-enzymatic mechanism as that which takes place in the brain.
Why It Matters:
This study represents a novel physiologic discovery with several potential implications, particularly if researchers can replicate it in humans.
First, population-level research has shown that diabetes is strongly associated with AD development, yet scientists do not know how the two were linked.
This finding suggests a hypothetical mechanistic connection between diabetes and AD. People with persistently high insulin levels, such as those with Type 2 diabetes, may have elevated levels of Aβ in their blood, which may throw off the balance of Aβ in the brain, eventually leading to plaque buildup. (The researchers note that other studies suggest that Aβ does increase in people with diabetes.)
Furthermore, measuring blood Aβ levels is a standard test for AD. But this research suggests that the amount of Aβ in circulation can vary considerably with blood-sugar levels (which are impacted by diet, among other things), meaning this may not be as reliable a test for AD as previously believed.