Member Profile
Who: Kevin Jubbal, 31
Where: Las Vegas
Time with Levels: Two Months
Most Useful Takeaway: Knowing that sleep is important is one thing. But understanding the effect that lack of sleep has on your body by seeing your blood sugar go out of control is a much more powerful motivator.
1. What was your health like before using Levels?
I was diagnosed with inflammatory bowel disease (IBD) in 2009 when I was 18. That’s when I really got into health optimization. And diet has been a big part of that experimentation. I’ve tried gluten-free, keto, plant-based, and others, all just trying to optimize my health and control my symptoms.
That’s been my central focus. Health is the number one thing when you have a chronic disease because if you don’t have your health when you’re flaring, nothing else matters. You don’t care about hanging out with your friends. You don’t care about how tasty food is. You don’t care about having fun. You just want to feel better.
That desire to prioritize my health has extended into things like trying to optimize my sleep, which relates to symptoms of autoimmune conditions, in addition to nutrition and other lifestyle factors. In pursuing health optimization, I’ve also landed on weight training and cycling for strength and cardiovascular fitness, respectively.
2. Why did you want to put a CGM on your arm?
I love experimenting and tweaking and trying to have a deeper understanding of my body’s processes. In addition to Levels, I’m constantly experimenting with other wearables, from sleep trackers and activity trackers to various tools to understand my metabolism or even my gut flora. With a family history of metabolic problems, notably pre-diabetes, I feel the urgency to be proactive.
Finally, IBD is an inflammatory process. When I’m optimizing my diet, there’s only so much you can do by following a protocol and checking your symptoms. If I can measure things such as blood glucose spikes because I know they won’t be good for my inflammation levels, I have something more objective to reference.
I wanted to figure out what is best for me because Western medicine management of IBD isn’t fully baked. Gastroenterologists will say that the literature suggests that diet doesn’t have an actual significant effect on the disease process. But if you ask a patient, they will say, ‘oh no, of course it does.’ And it makes sense. If we’re eating several pounds of foreign substance and our gastrointestinal system is interacting with it continuously, it would be shocking and highly counterintuitive for diet and nutrition not to play a significant role in our digestive processes. A CGM is one tool you can use to customize your diet because what works for one person isn’t always going to work for another person with IBD.
Learn more:
 3. What surprised you about the foods or eating habits that did or did not keep you stable?
3. What surprised you about the foods or eating habits that did or did not keep you stable?
One thing is eating late. I didn’t realize that because of melatonin inhibiting the secretion of insulin from the pancreas, if I have the same meal at 10 p.m. versus having it at 6 p.m., it will only spike glucose higher—and a lot longer. That reinforced to me that I should not eat late at night.
When I’m sitting down to eat, I have to be careful not to eat too fast. That’s a bad habit I have, but I think it resonates with people who are in careers where you have to scarf down food to get back to work quickly.
There’s also the order in which I eat. It makes sense that we get the salad as an appetizer before the carb-heavy entrée. Even with breakfast, I’ll focus on eating my vegetables and eggs before getting to my berries. You get the fiber first, which slows down the digestion of whatever is upstream, namely the carbohydrate-heavy foods.
And finally, I tend to practice time-restricted feeding. Six or eight hours is usually my feeding window. Sometimes I’ll do one meal a day, or OMAD. But I’ve found that it’s not ideal for my glycemic control when I do one meal because I’m eating so much in one sitting. For that reason, I try to eat a few smaller meals within my feeding window, or if I am going to OMAD, I’ll be more careful to reduce carbohydrates.
4. How have non-diet factors, such as exercise and sleep, influenced your blood sugar?
One of my favorite lessons was how cardio is one of the best cheat enablers. I found I could eat sweets right after an intense bout of cardio on my bike, and I wouldn’t spike. The takeaway here is that if I’m craving sweets, then I should save it for after I’ve earned it with a moderate- to high-intensity 90-minute bike ride.
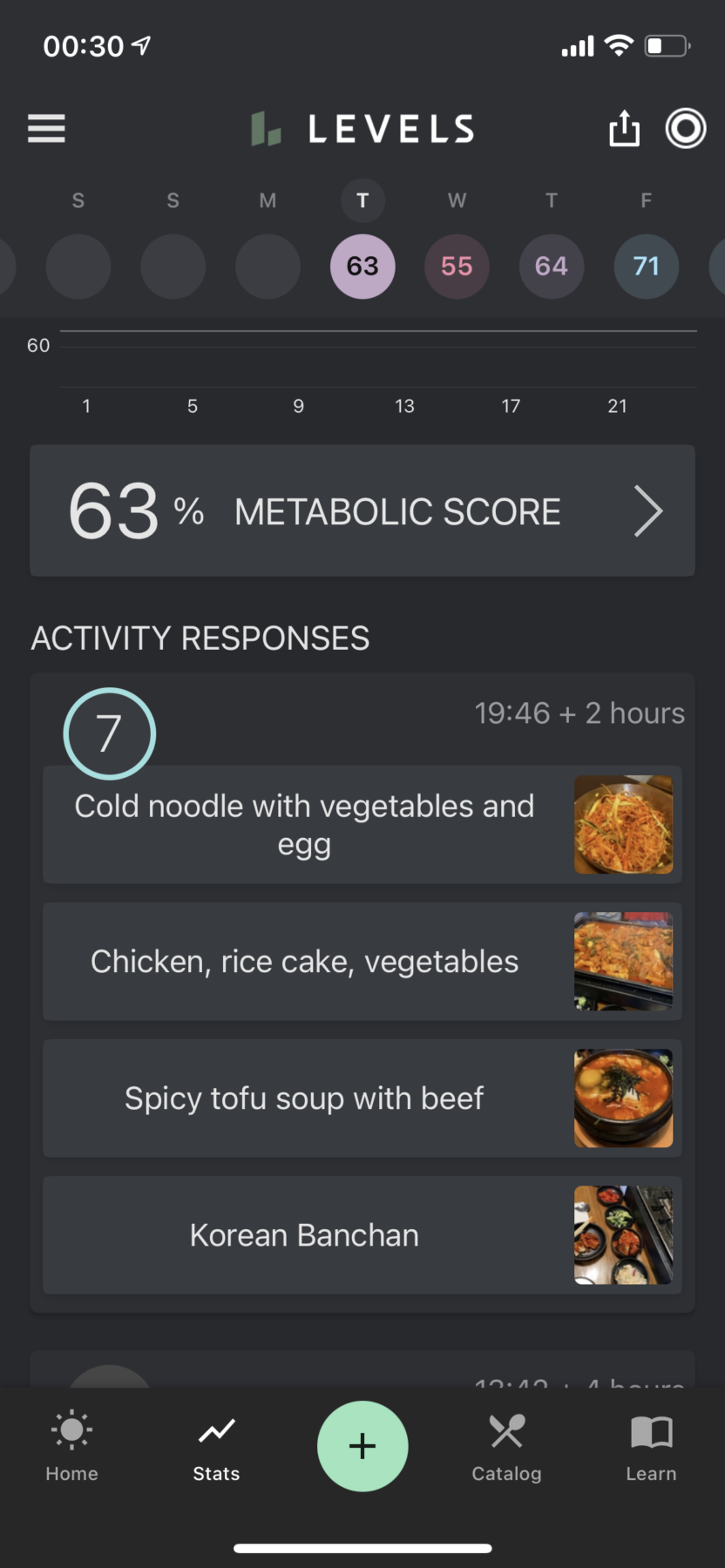
When I’m sleep-deprived, I’ll spike a lot harder, stay elevated for a lot longer, and see increased variability even at baseline without food. For example, I have my go-to’s when I order Thai from my favorite local restaurant. Despite having a similar meal each time, how high I spike is significantly influenced by what time I eat and how much sleep I got the night before.
A recent learning I had was how my infusions (part of my IBD treatment), which are a significant stressor on the body, also impact my ability to clear glucose. There are instances where I had the same meal (eating leftovers) before and after an infusion, and the glycemic response is night and day. This drives home the point that it’s not just a matter of the food we’re eating, but also the state of our body regarding stress, recovery, and related factors.
Ideally, what I could do is say, ‘I’m sleep deprived; therefore, I need to tighten up what I’m going to eat that day and avoid foods that can spike me.’ Sometimes I’m good about doing that. But I often find that when I’m sleep-deprived, I lack the discipline. The critical learning there is that I need to prioritize sleep. Matthew Walker’s book, Why We Sleep, is a great resource that has driven that point home for me.
Knowing that sleep is important is one thing. But understanding the effect that lack of sleep has on your body by seeing your blood sugar go out of control is a much more powerful motivator. That alone has helped motivate me to prioritize consistency and duration around my sleep habits.
5. What advice do you have for other people who might put on a CGM?
I talked to a friend about Levels at a conference, and she mentioned that wearing a CGM would make her feel very guilty and frustrated. I’m sure she’s not the only one to have that thought. I’d recommend using Levels as a tool in helping you learn more about yourself, not as something you can either succeed or fail at. It’s about learning more about your body and tweaking things. When you eat a meal and have a food coma, check what happened. I don’t want people to think, I spiked to this crazy number. I’m doomed. Instead, think about what you can learn from this. The key is to keep learning rather than assigning judgment to points in the learning process.
Learn more about Kevin Jubbal, MD, at kevinjubbal.com.


 3. What surprised you about the foods or eating habits that did or did not keep you stable?
3. What surprised you about the foods or eating habits that did or did not keep you stable?