I’ve suffered from migraines for more than 20 years. Like many migraineurs, the pain and frequency of my migraines increased during the pandemic. By November 2020, I’d gone from getting a migraine a few times a week to having one every single day. No amount of medication eased the pain, and as each excruciating day blurred into the next, I became desperate for relief.
After some digging, I found a book that stressed the importance of cutting back on carbs and sugar to prevent migraine attacks. I decided to give it a shot. To my surprise, within six weeks, I saw a dramatic improvement in my symptoms. I started going weeks at a time without a migraine, and when I did get one, it was far less severe than it had been in the past.
I didn’t realize it at the time, but I had taken a critical step in improving my metabolic health: By reducing the glucose load on my body, I’d decreased the role of insulin, which is closely linked to migraine.
What Are Migraines?
A migraine is not just a regular old headache—it is a disabling neurological disease that affects an estimated 12 percent of Americans (nearly 40 million people). In addition to a throbbing or pulsing sensation (usually on one side of the head), migraine sufferers may experience nausea, vomiting, sensitivity to light or sound, and aura (a visual disturbance like black dots, flashes of light, or zig-zags). Regular pain relievers rarely work—typically, we need prescription medication, such as a triptan or a CGRP inhibitor, and those too may not be effective or durable.
Migraines can last anywhere from a few hours to several days, and getting them more than 15 days a month is usually considered chronic migraine. Migraines are more than twice as common in women than men—indeed, 85 percent of chronic migraine sufferers are women (this may be due, in part, to monthly hormonal fluctuations).
“I learned how to take charge of my metabolic health—and in turn, take control of my migraines.”
The exact cause of migraine is unknown, but it’s thought to be a genetically inherited condition that occurs when overactive nerve cells trigger the release of substances that send pain signals to the brain, usually in response to changes in the external or internal environment. External triggers may include bright light, loud noises, or intense odors like strong perfume or cigarette smoke. Internal triggers may be anxiety, dehydration, specific foods, increased oxidative stress, or fluctuations in blood sugar.
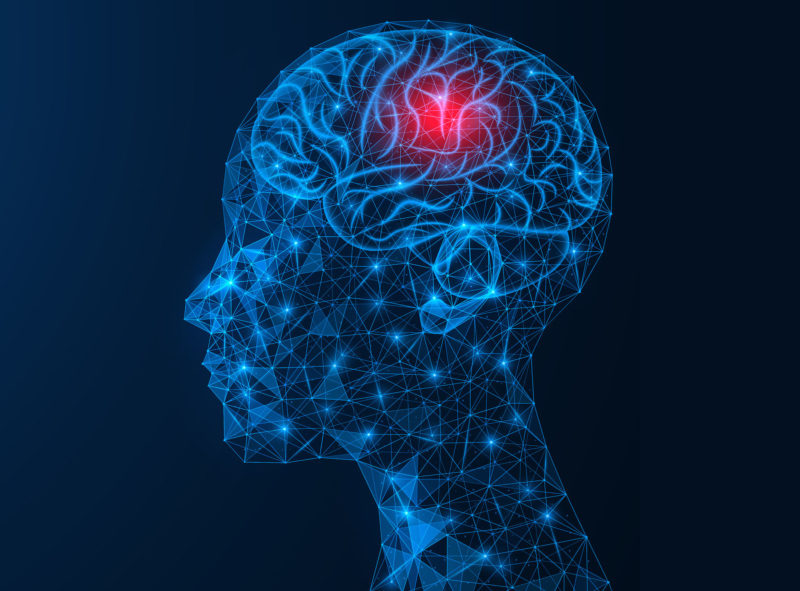
Migraine is a multifactorial condition, so there isn’t a single cause, nor is there a one-size-fits-all solution. There is evidence that migraine starts in the hypothalamus (an almond-size structure in the brain), which may provide insight into how to treat it. Indeed, functional brain imaging shows that the hypothalamus is teeming with activity before a migraine attack.
What’s the job of the hypothalamus? The hypothalamus keeps the body in homeostasis internally—it regulates temperature, blood flow, and energy availability. This means that certain kinds of disturbances—bright light, blood sugar fluctuation—may cause temporary hypothalamic dysfunction, resulting in a migraine attack. In short, migraineurs appear to have a more sensitive hypothalamus, so it’s not able to maintain homeostasis as well as a “normal” brain.
My Migraine Journey
I started getting migraines when I was 12, shortly after I got my first period. At first, over-the-counter meds like Advil helped (in middle and high school, I carried a bottle of the stuff in my backpack). But over time, the frequency and intensity of my migraines increased, and no amount of Advil (or Aleve or Excedrin) alleviated the pain.
I sought relief from every corner of healthcare: my primary care doctor, a neurologist, an allergist, a physical therapist, a chiropractor, and several acupuncturists. No one could help me in the long-term: The MDs incorrectly diagnosed me with tension headaches until I finally got a proper migraine diagnosis in my early 30s and prescribed meds that didn’t help. The acupuncturist and chiropractor provided short-term relief—I’d feel better for a few hours after treatment, but then the migraine would come roaring back.
I learned to live with migraines, but they took a toll. Being in chronic pain made it difficult to hold a 9-to-5 job. So I quit my full-time magazine editor gig and became a freelance writer so I could make my own schedule and lay down in a dark room with an ice pack on my head when a migraine struck. I frequently missed friends’ birthday parties and family gatherings because I was in bed with a migraine. Sometimes, when I didn’t want to miss an event, I’d push through the pain, but I always regretted it (there’s nothing worse than forcing a smile at a party when you’re in excruciating pain).
Living with chronic, worsening migraines became unbearable during the pandemic. There were times when I was in so much pain that I wanted to go to the hospital, but I couldn’t. The risk of contracting COVID-19 was too high, and the hospitals in New York City were already overflowing. But I was fortunate in the sense that I had the time and resources to find alternative solutions to my migraines. I learned how to take charge of my metabolic health—and in turn, take control of my migraines.
The Link Between Metabolic Health and Migraine
Over the last 20 years or so, researchers have found a strong association between insulin resistance and migraine. A recent review of 56 articles found associations between migraine and poor metabolic health, noting that “insulin sensitivity is clearly impaired in migraine.”
A study of middle-aged women in Italy—83 with episodic migraine, 83 with chronic migraine, and 83 with no migraine—found that women with chronic migraine were three times more likely to have insulin resistance than those with episodic migraine. Additionally, study participants with migraines (either chronic or episodic) were more likely to have metabolic syndrome, and obesity was associated with an increased risk of chronic migraines.
“It’s incredibly empowering to know that I can influence to some degree whether or not I get a migraine simply through my diet.”
Another study, conducted in Turkey, found increased insulin resistance in women with chronic migraine compared to women with episodic migraine and healthy controls. The researchers also found that migraineurs had higher levels of neuropeptide Y, a chain of amino acids in the nervous system that normally helps the body maintain homeostasis—too much of it, though, can have the opposite effect, throwing homeostasis out of balance.
In addition to insulin and glucose, there is also evidence that micronutrient deficiencies may contribute to migraine. Research has found associations between onset and treatment of migraine with vitamins D and B, magnesium, coenzyme Q10 (CQ10), alpha lipoic acid (ALA), and L-carnitine. The mechanisms vary but most are thought to be related to mitochondrial energy production, neuroinflammation, and oxidative stress. Vitamin B12 (riboflavin), for example, plays a role in the electron transport chain that turns oxygen to energy in the mitochondria, and studies have found that high doses of B12 can help prevent migraines. These micronutrients generally have limited side effects compared to other migraine drugs, so consuming more of these micronutrients via food or supplement may help provide migraine relief.

8 Micronutrients essential for metabolic health
Micronutrients are like tools that help our cellular machinery function better. Here's how they work, and how to ensure you're getting enough
Read the ArticleHow Insulin Resistance Impacts Migraine
Before diving into the specific mechanisms of how insulin resistance relates to migraine, it’s important to understand how hypothalamic dysfunction may play a role in migraine onset. Some research suggests that triggers related to the hypothalamus—such as hunger, temperature, erratic sleep, or other disturbances—may help initiate the series of events that trigger a migraine. There’s debate over the precise sequence of events, but researchers believe that networks in the trigeminovascular system (which is composed of cranial nerves) become dysfunctional and release chemicals that activate pain signals.
Researchers also aren’t entirely clear yet how insulin resistance fits into this migraine physiology, but here are some theories that have emerged from studies:
- Insulin overload: A study in men and women found that insulin levels were significantly higher in migraineurs compared with healthy controls. The study authors hypothesize that insulin itself may be to blame—it may not be functioning correctly in the hypothalamic and limbic regions of the brain and the brainstem. Additionally, insulin may stimulate the release of hormones (such as gonadotropins, which are responsible for the secretion of reproductive hormones) known to trigger migraines. It’s also important to note that the brain is an insulin-sensitive organ: Insulin receptors are abundant in the brain, and insulin action produces behavioral and metabolic effects within the central nervous system. Interestingly, a recent study found that when frequent migraineurs were treated with alpha-lipoic acid, an insulin-sensitizing supplement, they experienced a significant reduction in migraine frequency.
- Oxidative stress: Your body’s energy-generating processes produce molecules called reactive oxygen species (ROS), which can be damaging if they react with cells or tissue. This is known as oxidative stress and is usually kept in check by antioxidants, which neutralize ROS. Growing research indicates that this oxidative stress and a deficit in antioxidants such as ALA could be behind migraines (which may account for the positive effect of ALA in the above study). The theory is that many of the triggers of migraine cause oxidative stress and that migraineurs may have an added sensitivity through specific channels in the brain to detect this oxidative stress.
- Obesity: Insulin resistance is associated with obesity, and research shows that obesity significantly increases the risk of migraines. A recent meta-analysis showed that people with obesity had a 27 percent increased risk of migraine compared to those at a normal weight. Hormones called adipokines (which are made by adipose tissue, or fat) may play a role, as they regulate appetite and satiety, sensitivity to insulin, and inflammatory response. Obesity is also correlated with high levels of calcitonin gene-related peptide (CGRP), a chemical that can initiate migraine. Some of the latest migraine drugs, including Emgality, Aimovig, and Ajovy, block CGRP receptors to stop a migraine before it starts.
- Increased nitric oxide stress: Research shows that hyperinsulinemia (often the driver and result of insulin resistance) is correlated with increased nitric oxide stress, a known trigger of migraine attacks. Nitric oxide plays a pivotal role in regulating the nervous system—specifically, the trigeminovascular system, which researchers believe is involved with headaches. It’s also correlated with pain processing, which may help explain its association with migraines.
- Elevated neuropeptide Y (NPY) levels: NPY is a protein complex that plays a role in food intake and pain processing. A recent study found that migraineurs have significantly higher NPY levels. The study authors hypothesize that migraines activate the sympathoadrenal system, which helps regulate the body’s response to outside stimuli (like food and glucose, for example), and that this may lead to increased NPY levels. NPY is known to be associated with insulin resistance, but the causal direction is still unclear.
A Path Forward: Preventing Migraine by Reducing Glucose
For me, reducing carbs and sugar has led to a significant reduction in migraine frequency and pain. Given the research, it makes sense that decreasing my glucose load has lowered the risk of a migraine attack—and likely helped me avoid insulin resistance.
Today, I mainly adhere to a ketogenic (keto) diet, a low-carb, high-fat, moderate-protein way of eating. Eating fewer carbs puts the body in a metabolic state called ketosis, where the body relies on fat (instead of carbs) for fuel. Using fat as my primary fuel source helps my hypothalamus maintain energy constancy—I experience minimal fluctuations in my energy levels, appetite, and mood.
Researchers are at the beginning stages of understanding how a keto diet helps migraineurs, but the research is promising (previous studies on the keto diet centered around another neurological disease—epilepsy—and found it to be highly effective).
In a recent study conducted in Italy, researchers analyzed 35 migraineurs who were overweight or obese. The participants alternated between eating a low-calorie ketogenic diet and a low-calorie non-ketogenic diet for one month. The results showed a significant decrease in migraines during the month that participants ate a low-calorie keto diet. The researchers hypothesize that the improvement is due to ketones (more than the weight loss) but say that more research is needed to see how keto would impact non-obese people. (When you reach ketosis through a reduction in carbs, ketones are produced by the liver.)
Ever since I adopted a keto diet in November 2020, I’ve experienced a vast improvement in my migraines. I’ve gone from getting a migraine 20 to 25 days a month to maybe four or five times a month. I’ve also made significant changes to my lifestyle: I go to sleep and wake up at the same time every day, work out several times a week, and do transcendental meditation to manage stress (all steps that help regulate my hypothalamus). When it comes to a complex disease like migraine, this sort of multi-pronged approach is crucial.
It’s incredibly empowering to know that I can influence to some degree whether or not I get a migraine simply through my diet. Instead of living in fear that a migraine will ruin my day (or my week), I now have the power to keep the attacks from coming. In other words, I control my migraines—they no longer control me.