Vimal Ramjee, MD FACC
Cardiologist & Consultant
Director, Cardiovascular CT Program, Memorial Hospital
AI Clinical Specialist, ACC National Digital Health Analytics Workgroup
Executive Coach, VentureWell
Heart Disease in on the Rise
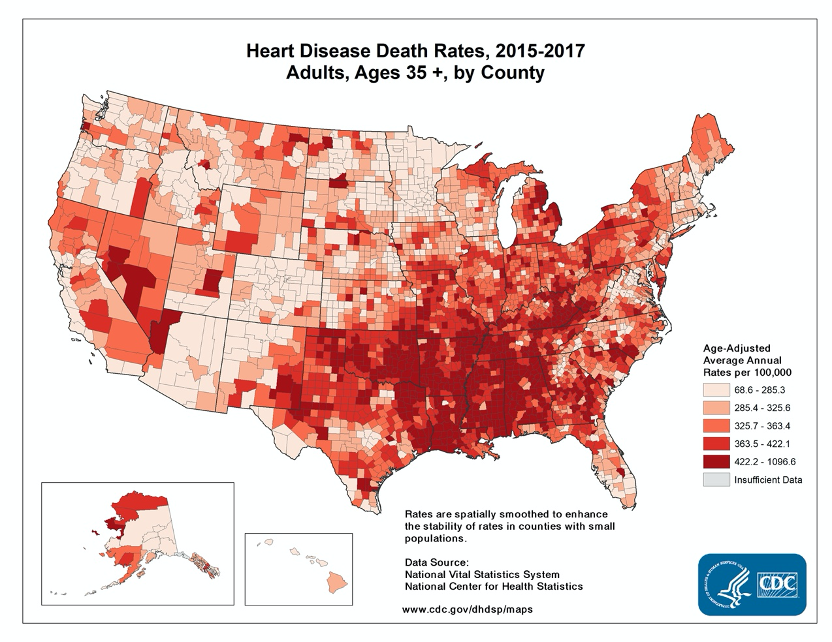
Heart disease is the most prevalent and burdensome illness worldwide. A remarkable 25% of deaths in the United States are directly a result of cardiovascular disease (see Figure 1, CDC) [1]. As a cardiologist practicing in the hotbed of heart disease — the ultra-high prevalence Southeastern US — I regularly take care of people who have a spectrum of complex cardiac and vascular problems. In my daily practice of leveraging cutting-edge medical technologies to get patients better from heart attacks, valve disease, heart failure and the like, I often contemplate how they could have changed their outcome and perhaps circumvented disease or death altogether.
The answer lies in plain sight: less sugar and fewer processed carbohydrates.
Sugar and Processed Carbohydrates Drive Heart Disease
We live in a world of overeating and undernourishment. Most of the food products marketed to us by the food industry are intentionally engineered to hit a ‘blisspoint’ (greatest palate pleasure) to serve the primary objective of generating revenue, but not wellbeing [2]. As a result, the majority of what we eat in the modern day in the Standard American Diet (aka SAD) — comprised of biologically foreign “food-like” products — is energy dense and nutrient poor [3]. Because sugar has remarkable biochemical properties that make it several times more biologically addictive than cocaine, it is the central ingredient that food companies use in their products to keep consumers coming back, perhaps out of their own volition [4–8]. Sugar results in a marked dopamine surge in our brain, similar to most drugs of abuse [5,7,8,9]. As abundant as sugar is, with the average American now consuming an equivalent of 22 teaspoons a day (much of which is hidden), the adverse health implications are astounding and second to none.
“A remarkable 25% of deaths in the United States are directly a result of cardiovascular disease.”
Despite concerted efforts from the food industry to detract from the detrimental effects of their prime ingredient through lobbying, coercion, fraudulent practices, and consumer confusion tactics, sugar and processed carbohydrates (a sugar equivalent) have emerged as pinnacle drivers of modern day disease via the principal mechanism of inflammation [10–13]. Robust scientific studies have shown a multitude of deleterious effects from sugar and processed carbohydrate products, including, but not limited to:
- 30% higher risk of death from cardiovascular events (heart attacks, strokes, heart failure) [14].
- Increased risk of impaired glucose tolerance, prediabetes and diabetes [14–16].
- Increased risk of hypertension [17].
- Worsening of cholesterol levels (increased LDL and oxLDL, increased triglycerides, decreased HDL) [14,18,19].
- Increased risk of obesity [14,16,20].
How Sugar Damages our Bodies
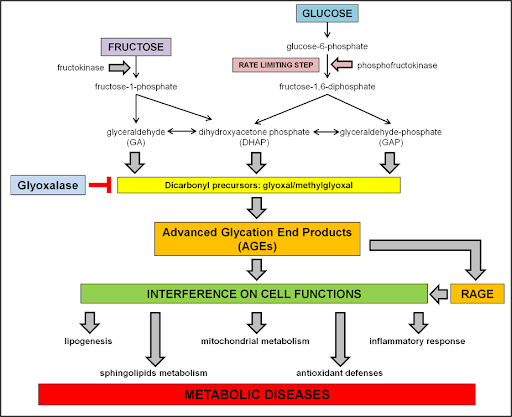
The role of dietary sugar and its precursor (carbohydrates) in the pathogenesis of disease is so vast that it has grown into a distinct and booming field of study called glycobiology [21]. Sugar and processed carbohydrates create disease as a result of multiple biological mechanisms (see Figure 2) [19]. It is well known that dietary sugar gives rise to toxic endogenous chemicals called advanced glycation end-products (AGEs) [19,22]. These by-products are directly damaging to multiple organ systems, including blood vessels, muscle, liver, brain and heart tissue, among others [22]. At the cellular level, dietary sugar gives rise to inordinate mitochondrial dysfunction and oxidative stress [23,24]. An emerging scientific trend now shows that dietary sugar fragments, also known as glycans, directly affect how our immune system is calibrated and may contribute to inflammation [25–27]. Considering the vast array of systems affected, it is no surprise that diabetes and obesity are approaching prevalence rates that affect 1 out of every 2 people in the United States [28,29].
Addressing Risk Factors to Avoid a Heart Attack
We have known that optimizing and addressing conventional risk factors is crucial to reducing future heart attacks, strokes and the like. These risk factors — hypertension, high cholesterol, obesity, diabetes, smoking, and physical inactivity — have been identified as long as 100+ years ago [30–33]. Although there have been notable strides in medical therapies to target some of these risk factors, the growing prevalence of heart disease remains disconcerting and underscores the need to address individual risks at an earlier stage.
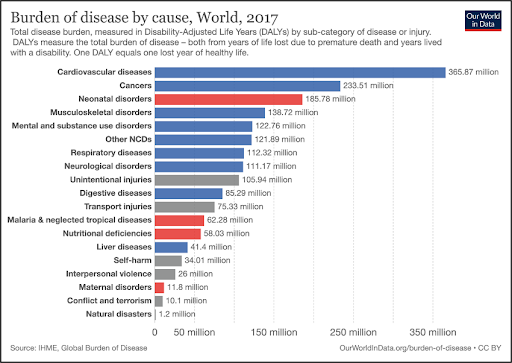
In concert with this need, a new era of medicine wherein prevention is emphasized has taken centerstage. New tools and the advent of digital health is giving rise to novel, often more effective strategies in disease prevention. This is precisely where continuous glucose monitoring (CGM) technology adds major value. Knowing that unaddressed impaired fasting glucose gives way to prediabetes, which consequently progresses to diabetes, it stands that earlier use of CGM technology for at risk but not yet diagnosed diabetes holds the potential to significantly curb the future worldwide burden of cardiovascular and metabolic disease (see Figure 3) [34,35]. If you can put out the flame before the full house burns down, then why wait?
In the current state of medicine, patients may get annual or biannual lab draws, which at best quantify a fasting glucose level and hemoglobin A1c (HbA1c). While these two biomarkers may provide some insight into an individual’s overall glucose control, they hardly scratch the surface and are often late stage findings when abnormal. CGM technology allows for streamlined, real-time feedback of your personal metabolic response to everything you ingest in the context of your daily life. CGMs allow for active prevention: intentional directed lifestyle modifications that are personalized to you, based on objective data points, and implemented over long periods of time. It provides many layers of information above and beyond that of point-of-care blood draws, and in doing so, helps to facilitate true behavior change specific to you and your lifestyle. Some of the key concepts a CGM wearable brings to light include deeper understanding that:
- Sugar sweetened products are extremely detrimental for your metabolic and heart health.
- Processed foods — typically very high in the carbohydrate macronutrient — generate similar glucose surges to sugar in the body otherwise unbeknownst to you.
- Many health-marketed food products (e.g. bars, drinks, yogurts, granola, supplements, smoothies, energy boosters) are extremely high in sugar, sugar analogs and processed carbohydrates. They are often the source of low energy levels due to marked insulin-glucose fluctuations.
- Real food is incredibly gentle on our body from a metabolic standpoint, much of which is due to a complex and healthy balance of macronutrients (fat + protein + fiber + natural sugar).
- The timing of a meal as it pertains to your physical activity remarkably alters the metabolism of what you eat.
- Lifestyle factors like stress, work, and sleep, among other factors, play a larger role in your metabolic health than you would think.
So what does this all add up to? Stop letting the food industry and modern day eating culture hijack your brain into a vortex of dopamine to generate profits for a self-seeking industry [3,8,11,36,37]. Be careful and be intentional about what you eat — look at labels from an analytic standpoint. In the confusing world of mainly processed foods, “superfoods” “natural” foods, and “health” foods, there is no better way than a CGM wearable to understand how your body is interacting with what you eat and to optimize your wellbeing.
While cardiovascular disease represents the nexus of multiple lifetime risk factors, sugar and processed carbohydrates are key unifying drivers of inflammation that underlie many of the cardiac risks we target in clinical practice [14–17,38–40]. If you are able to effectively use a CGM to circumvent these dangerous players and proactively protect your metabolic health, you may have found your ticket out of a possible future heart attack.
About the Author
Dr. Ramjee is a Senior Staff Cardiologist and the Director of Cardiovascular CT at the Chattanooga Heart Institute with Memorial Hospital. He is quintuple board-certified in Cardiovascular Disease (Cardiology), Echocardiography, Nuclear Medicine, Cardiac CT, and Internal Medicine. Dr. Ramjee leverages high-level expertise in cutting-edge technologies to help repair the heart with a minimally-invasive, needle-only approach. As a member of the national ACC Digital Health Analytics Workgroup, he also creates proprietary clinical AI and machine learning solutions for forward-thinking health-oriented businesses. He specializes in cardiovascular imaging, general cardiology, and structural imaging. He has been featured in FOX News, NBC Morning Show, and Cardiovascular Business Magazine.
References
- CDC. Heart Disease Facts | cdc.gov. Centers for Disease Control and Prevention. Published June 22, 2020. Accessed August 26, 2020. https://www.cdc.gov/heartdisease/facts.htm
- Moss M. The Extraordinary Science of Addictive Junk Food. The New York Times. https://www.nytimes.com/2013/02/24/magazine/the-extraordinary-science-of-junk-food.html. Published February 20, 2013. Accessed August 26, 2020.
- Fuhrman J. The Hidden Dangers of Fast and Processed Food. Am J Lifestyle Med. 2018;12(5):375-381. doi:10.1177/1559827618766483
- Lenoir M, Serre F, Cantin L, Ahmed SH. Intense Sweetness Surpasses Cocaine Reward. PLoS ONE. 2007;2(8). doi:10.1371/journal.pone.0000698
- Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: Behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32(1):20-39. doi:10.1016/j.neubiorev.2007.04.019
- Madsen HB, Ahmed SH. Drug versus sweet reward: greater attraction to and preference for sweet versus drug cues. Addict Biol. 2015;20(3):433-444. doi:10.1111/adb.12134
- Schulte EM, Avena NM, Gearhardt AN. Which Foods May Be Addictive? The Roles of Processing, Fat Content, and Glycemic Load. PLOS ONE. 2015;10(2):e0117959. doi:10.1371/journal.pone.0117959
- Small DM, DiFeliceantonio AG. Processed foods and food reward. Science. 2019;363(6425):346-347. doi:10.1126/science.aav0556
- Rada P, Avena NM, Hoebel BG. Daily bingeing on sugar repeatedly releases dopamine in the accumbens shell. Neuroscience. 2005;134(3):737-744. doi:10.1016/j.neuroscience.2005.04.043
- Kearns CE, Schmidt LA, Glantz SA. Sugar Industry and Coronary Heart Disease Research: A Historical Analysis of Internal Industry Documents. JAMA Intern Med. 2016;176(11):1680. doi:10.1001/jamainternmed.2016.5394
- Stuckler D, Nestle M. Big Food, Food Systems, and Global Health. PLoS Med. 2012;9(6). doi:10.1371/journal.pmed.1001242
- Tempels T, Verweij M, Blok V. Big Food’s Ambivalence: Seeking Profit and Responsibility for Health. Am J Public Health. 2017;107(3):402-406. doi:10.2105/AJPH.2016.303601
- Nestle M. Food Lobbies, the Food Pyramid, and U.S. Nutrition Policy. Int J Health Serv. 1993;23(3):483-496. doi:10.2190/32F2-2PFB-MEG7-8HPU
- Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. Added Sugar Intake and Cardiovascular Diseases Mortality Among US Adults. JAMA Intern Med. 2014;174(4):516-524. doi:10.1001/jamainternmed.2013.13563
- Howard BV, Wylie-Rosett J. Sugar and Cardiovascular Disease: A Statement for Healthcare Professionals From the Committee on Nutrition of the Council on Nutrition, Physical Activity, and Metabolism of the American Heart Association. Circulation. 2002;106(4):523-527. doi:10.1161/01.CIR.0000019552.77778.04
- Vos MB, Kaar JL, Welsh JA, et al. Added Sugars and Cardiovascular Disease Risk in Children: A Scientific Statement From the American Heart Association. Circulation. 2017;135(19). doi:10.1161/CIR.0000000000000439
- DiNicolantonio JJ, Lucan SC. The wrong white crystals: not salt but sugar as aetiological in hypertension and cardiometabolic disease. Open Heart. 2014;1(1):e000167. doi:10.1136/openhrt-2014-000167
- Welsh JA, Sharma A, Abramson JL, Vaccarino V, Gillespie C, Vos MB. Caloric Sweetener Consumption and Dyslipidemia Among US Adults. JAMA. 2010;303(15):1490-1497. doi:10.1001/jama.2010.449
- Aragno M, Mastrocola R. Dietary Sugars and Endogenous Formation of Advanced Glycation Endproducts: Emerging Mechanisms of Disease. Nutrients. 2017;9(4):385. doi:10.3390/nu9040385
- Aller EEJG, Abete I, Astrup A, Martinez JA, Baak MA van. Starches, Sugars and Obesity. Nutrients. 2011;3(3):341-369. doi:10.3390/nu3030341
- Varki A, Kornfeld S. Historical Background and Overview. Cold Spring Harbor Laboratory Press; 2017. doi:10.1101/glycobiology.3e.001
- Goldin Alison, Beckman Joshua A., Schmidt Ann Marie, Creager Mark A. Advanced Glycation End Products. Circulation. 2006;114(6):597-605. doi:10.1161/CIRCULATIONAHA.106.621854
- Kim Jeong-a, Wei Yongzhong, Sowers James R. Role of Mitochondrial Dysfunction in Insulin Resistance. Circ Res. 2008;102(4):401-414. doi:10.1161/CIRCRESAHA.107.165472
- Cunarro J, Casado S, Lugilde J, Tovar S. Hypothalamic Mitochondrial Dysfunction as a Target in Obesity and Metabolic Disease. Front Endocrinol. 2018;9. doi:10.3389/fendo.2018.00283
- Cobb BA, Kasper DL. Coming of age: carbohydrates and immunity. Eur J Immunol. 2005;35(2):352-356. doi:10.1002/eji.200425889
- Marth JD, Grewal PK. Mammalian glycosylation in immunity. Nat Rev Immunol. 2008;8(11):874-887. doi:10.1038/nri2417
- Sugar-coated world: Probing the mysteries of glycan structure and function. ScienceDaily. Accessed August 24, 2020. https://www.sciencedaily.com/releases/2017/12/171218120356.htm
- Overweight & Obesity Statistics | NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed August 26, 2020. https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity
- CDC. Obesity is a Common, Serious, and Costly Disease. Centers for Disease Control and Prevention. Published June 29, 2020. Accessed August 26, 2020. https://www.cdc.gov/obesity/data/adult.html
- Ramjee V, Sperling LS, Jacobson TA. Non-high-density lipoprotein cholesterol versus apolipoprotein B in cardiovascular risk stratification: do the math. J Am Coll Cardiol. 2011;58(5):457-463. doi:10.1016/j.jacc.2011.05.009
- Fiuza-Luces C, Santos-Lozano A, Joyner M, et al. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol. 2018;15(12):731-743. doi:10.1038/s41569-018-0065-1
- Understand Your Risks to Prevent a Heart Attack. www.heart.org. Accessed August 26, 2020. https://www.heart.org/en/health-topics/heart-attack/understand-your-risks-to-prevent-a-heart-attack
- Harold on History | Historical Perspectives on Hypertension. American College of Cardiology. Accessed August 26, 2020. http%3a%2f%2fwww.acc.org%2flatest-in-cardiology%2farticles%2f2017%2f11%2f14%2f14%2f42%2fharold-on-history-historical-perspectives-on-hypertension
- Weyer C, Bogardus C, Mott DM, Pratley RE. The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J Clin Invest. 1999;104(6):787-794. doi:10.1172/JCI7231
- Gastaldelli A, Gaggini M, DeFronzo RA. Role of Adipose Tissue Insulin Resistance in the Natural History of Type 2 Diabetes: Results From the San Antonio Metabolism Study. Diabetes. 2017;66(4):815-822. doi:10.2337/db16-1167
- James C. Junk food, junk science? Science. 2018;362(6410):38-38. doi:10.1126/science.aau6602
- Isganaitis E, Lustig RH. Fast Food, Central Nervous System Insulin Resistance, and Obesity. Arterioscler Thromb Vasc Biol. 2005;25(12):2451-2462. doi:10.1161/01.ATV.0000186208.06964.91
- Buyken AE, Flood V, Empson M, et al. Carbohydrate nutrition and inflammatory disease mortality in older adults. Am J Clin Nutr. 2010;92(3):634-643. doi:10.3945/ajcn.2010.29390
- Giugliano D, Ceriello A, Esposito K. The Effects of Diet on Inflammation: Emphasis on the Metabolic Syndrome. J Am Coll Cardiol. 2006;48(4):677-685. doi:10.1016/j.jacc.2006.03.052
- Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Nature. 2017;542(7640):177-185. doi:10.1038/nature21363