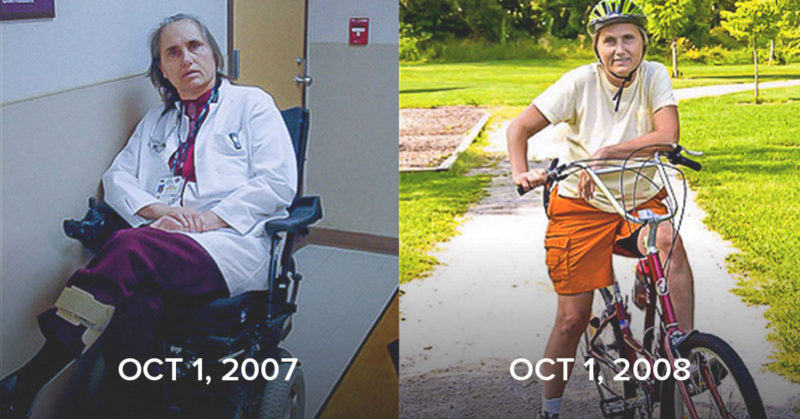
Dr. Terry Wahls is a clinical professor of medicine at the University of Iowa and also maintains a prolific research career. She’s had more than 60 peer-reviewed scientific abstracts, posters, and papers. Her personal story is incredible: More than 20 years ago, she was diagnosed with multiple sclerosis, an autoimmune disease that had her using a wheelchair and on a path towards being bedridden. She took her health into her own hands, scouring the literature to understand if there were any possible treatments for MS. She ultimately developed the Wahls Protocol, which is the nutrition and lifestyle program to treat chronic autoimmune diseases. It reversed her disease process, restored her health, and allowed her to get back on her feet (and her bike!).
Her learnings turned into an incredible book called The Wahls Protocol. She gave a TEDx talk that has over 3.5 million views on YouTube called Minding your Mitochondria. She’s inspired countless individuals to make the choices to support their health and vitality.
Levels chief medical officer Dr. Casey Means interviewed Dr. Wahls for a recent episode of A Whole New Level. Below is an edited version of that conversation.
On the experiences that led her to develop the Wahls Protocol
Terry Wahls: When I was in medical school, a few years ago, we were taught that autoimmune diseases are the immune cells attacking themselves. We don’t really know why. They, for reasons entirely unknown, must be genetic. At that point, we didn’t even link infections. All we had was prednisone. Then we started adding some other immune-suppressing drugs. [Our understanding became] a little bit more sophisticated. But we appreciate that there are hundreds of genes that increase the risk. There’s still this long list of unknown environmental factors. The conventional approach still focuses entirely on immune suppression. Of course, that’s not the approach that I take, nor is it the approach that I teach. I focus on all the modifiable lifestyle factors that we can address. We focus on creating health, and as a byproduct, you may discover that your chronic diseases begin to get under better control and then begin to regress.
I’m going to take it back to my health journey here for a little bit. Forty years ago, during medical school, I started having these electrical face pains. They build over a period of the next seven years. I had an episode of visual dimming—seeing a neurologist can’t explain that. Fortunately, they don’t connect my face pain and visual dimming because they could have diagnosed MS then. Fortunately for me, they did not. Thirteen years later after, I had my two kids. Then I developed leg weakness. See the best people, take the newest drugs. Within three years, I’m in a tilt and recline wheelchair. And that’s when I decided, “You know what, it’s pretty clear I’m going to become bedridden, demented.” The trajectory of my face pain is such that it’s more frequent, more severe, far more difficult to turn off. I’m already on a maximum dose of meds. I’m already going to the pain clinic. We’ve already gone to multiple pain centers.
I am likely to have my face pain turned permanently on. At that point, light, sound triggers my pain, speaking triggers my pain, swallowing triggers my pain. I’m taking a high dose of Solu-Medrol when these episodes turn up. I’m like, “Okay, I’ve got young kids. I have to do everything that I possibly can.” So, I can still read. I went to PubMed, and I started reading the basic science. At first, I was looking for drug development studies, then I had this big “Aha”—I can’t get these drugs. I switched over to start reading nutraceutical studies and started with a supplement cocktail. I created this supplement cocktail. I was focusing on cognitive decline, Alzheimer’s, Huntington’s disease, ALS because the nature of my disease had been a slow progression, looked much more like a progressive MS. Even though I’d had two relapses in my entire, at that point 27-year, history of my disease.
It appeared to me that the root problem was mitochondria. They couldn’t make enough energy. My supplement cocktail was focused on mitochondrial nutraceuticals. After six months I was no better. I was pissed off, and I stopped the model. I couldn’t get up, couldn’t go to work. After the third day, my wife Jackie says, “Honey, why’d you take the supplements again. I mean, what’s it going to hurt?” So, I take them, and the next day I can get up and I can go to work. Now mind you, I’m still struggling with fatigue, but I’m like, “Oh, my God, that was really cool.” Two weeks later I do the same thing. I stopped my supplements. Wait three days, start them up the third day, and I can pop back up and go to work.
Now mind you, popping up is hardly popping that much, but I could at least go to work. And I was like, “This was empowering. Oh, my God, there is something to this.” Now I am really excited about reading the literature. Every day I’m scanning and reading a paper or two after my family’s gone to bed. I’m still okay with thinking that I can get by with four to five hours of sleep a night. I spend my time reading, realizing that was probably not a very smart thing to be doing. For years, I’m really focused on fixing my mitochondria with supplements. I got a gradually more complicated supplement cocktail and I find IFM, take their course on functional medicine, have a little deeper understanding of a longer list of supplements. Then a couple of months later, I had this really big “Aha” because I’d already switched from being vegetarian to a paleo diet based on Loren Cordain’s work and his papers.
I had this idea: What if I took this long list of supplements and said, where are they in the food supply? And I got them from the food? It was the first decision that I said, “I’m going to focus on creating health.” That was more research that I had to do, and the Linus Pauling Institute on Micronutrients was very helpful. They helped me identify the food sources. In the early days, I had this long list of foods that were stressing my diet. This new focus started on December 26. Within a month, I was not as exhausted and my physical therapist said, “Terry, you’re getting stronger.” He began to advance my exercises. Within three months I did this really radical thing: I get out of my wheelchair, walked down the hall, and mailed a letter, and my colleagues are like, “Oh, my God, Dr. Wahls, you’re walking! You’re walking!” And that’s stunning. About four months after that I decided I want to try bike riding again.
We have this emergency family meeting. It’s on Mother’s Day. We decided that I can try riding my bike. My son’s going to jog alongside on the left, my daughter Zeb is going to job alongside on the right. And Jackie’s going to follow on her bike. I push off, it wobbles a little bit, but I catch my balance and I’m biking, and my kids are crying, Jackie’s crying, I’m crying. If you look at my eyes closely, you see I’m crying, reliving that moment because that’s when I figured out—up until then, as part of the adaptation to living with a progressive neurodegenerative disease, you let go of the future. You take each day as it unfolds. So even though I was remarkably better walking around the neighborhood, I was still taking each day as it unfolded. All of my physicians for seven years had said, “You’ve got secondary-progressive MS, functions once lost will never come back.”
I didn’t know what was happening. I knew that day by day, but today I rode my bike. I knew that the current understanding of MS was incomplete and that who knew how much recovery might be possible. Four months after that, I do an 18.5-mile bike ride with my family. Once again, we’re all crying. My kids are crying, my wife’s crying, and I’m crying when I finished that bike ride. That really transformed how I thought about disease and health, and that transformed the way I practice medicine. It would transform my mission in life and the way I conduct my research.
Casey Means: I’m bowled over. And I am just so grateful to you for the work that you put in to dig deeper and to challenge the convention and go to some of the preclinical research, the mouse research and actually put together a whole new framework for thinking about health that was really based on systems biology and around giving the cells what they need to function properly.
On “creating health” rather than treating disease
Terry Wahls: This was all about thinking about the cells. Once I zeroed in on, “Okay, the mitochondria, I’ve got the nutrition right for the mitochondria.” Of course, I was thinking supplements—all the supplement cocktails—which got complicated. Nobody was talking about the microbiome yet. Because we didn’t know about that. It’s sort of embarrassing now to realize how long it took me to think, “Okay, I have made some dietary changes that were important, but what if I structured, instead of thinking about what to avoid, what I should be eating and I could use all these things that I said were good for mitochondria, figure out where they the food supply and probably other really important molecules would come along as well.” I want everyone to know that I did not get better from that supplement cocktail. People have heard about my use of electrical stimulation muscles. I did not recover. As much as I love e-stim, I did not recover.
The magic was when I shifted my thinking to creating, “Hell, am I doing everything that I can? Have I maximized my nutrition using food to the very best that I possibly can have?” I got back to meditation. I had to; we did that. I always stayed on the exercise bandwagon. I could choose to work very hard with my physical therapist, but it’s the creation of health. When we focus on treating disease, we get it wrong. Even when we focus on those mouse model preclinical studies, we’re still going to get those wrong because they’re focused on understanding pathology, one molecular pathway, and health and life are deeply interconnected. All of those metabolic pathways are so richly interconnected with checks and balances that when we focus on pathology, we will not be able to correct health. But if we focus on health, on all the things that underpin health, and add that incremental step, that’s when the magic happens for me. That’s when the magic happens in the patients I take care of.
Casey Means: You really got me started on thinking that we have to focus on the cell—which now is the dominant way I view health and medicine. All health and disease come from either cellular function or cellular dysfunction. This is one of the basic building blocks of our bodies. Obviously, there’s the atomic level as well, but these are these beautiful machines that are working so hard, but they need specific things to function properly. They need the avoidance of other things to function properly. And that’s where that really beautiful relationship between food and the cell comes into play. Because like you said, supplements may have a few of these things that the cell needs, but food has thousands of chemicals that we don’t even know that give this beautiful machine what it needs to generate health for us.
But I think a point that you make that is so important is that when we focus on real, whole, cleanly grown foods, we’re fighting most of the battle here. We’re getting thousands and thousands of chemicals in plants that are going to do such good work for ourselves.
Terry Wahls: I believe that number’s actually about 80,000 constituents. It’s unbelievable. And that’s in plants. Then it will go into the animal protein and to the fungi as well. That number becomes even larger. If we think about our ancestral beginnings, whether we go back as Homo sapiens 250,000 years, or we diverge from the primates six million years, or when we became mammals 200 million years when we were unicellular, which are now billions of years, we had this very long history of metabolic complexity. That means that the solution isn’t going to be a single molecule drug-based solution. We have to honor the complexity of our chemical pathway.
On the importance of maintaining mitochondria
Casey Means: I’d love to pick your brain about the mitochondria. Why can mitochondrial dysfunction lead to the body attacking itself in autoimmune disease? What’s the pathway between problems with our mitochondria, which, unfortunately, the Western and modern lifestyle in many ways are hijacking and making dysfunctional?
Terry Wahls: I might be incorrect here, but I see it more as an accelerant that if your mitochondria cannot generate energy efficiently, then whatever disease processes you have will be accelerated. I think the mitochondrial dysfunction is really an accelerant. Not enough energy puts all of these tissues in strain, and it will accelerate the disease process. In addition, because of the cell danger response, we now know the mitochondria are deeply involved in recognizing cell danger. When the inner contents spill out into extracellular space, those molecules, particularly ATP, are recognized by the cell membranes and that activates the innate immune system. And then that will address the pathogen, the infection, or, as in when I broke my wrist, the fracture and cleans up the debris. In the second step, the mitochondria call in the stem cells to do the repair work. And [they’re involved in] the third step, which is reintegrating the repaired tissues back into the surrounding tissues so they can function normally and complete healing and resolve the inflammation.
The mitochondria are involved in all three of those steps. It’s both an accelerant and intimately involved in immune function. And either accelerating immune function or failing to resolve the immune dysfunction. It has dual roles. I think it’s a very big player in autoimmunity. But it’s also a very big player in most of our non-infectious chronic disease states, whether it’s a mental health problem, obesity, diabetes, cardiovascular disease.
On the role of diet and blood sugar in autoimmune disease
Casey Means: You’ve done quite a bit of clinical research in the MS population and have looked at several biomarkers in your research of metabolic health in this population. What do you see in your own dataset in terms of rates of increased blood sugar or insulin resistance or metabolic dysfunction in a population with MS versus a non-autoimmune control population?
Terry Wahls: That’s a very consistent finding across most autoimmune disease states, whether it’s MS, lupus, RA, and it’s probably true for psoriasis. Although I don’t know, I certainly predict that of the hundreds of autoimmune diseases they’ll probably have 1.5 to 2.5 times the rate of the general population of insulin resistance and metabolic syndrome.
Casey Means: What do you think is going on here in terms of the mechanisms?
Terry Wahls: We have wandered so far from our evolutionary roots. The diet we eat is so radically different. We eat continuously. We eat a lot of sugar. We eat a lot of fructose. We eat a lot of high glycemic index foods. We are continuously forcing the release of insulin. We have disrupted our microbiome. We are eating so many synthetic compounds in our diet, putting them on our skin. All of those factors will drive insulin resistance. All of those factors increase our vulnerability to autoimmunity. All of those factors increase our vulnerability to serious mental health problems in chronic disease states. I think the root cause is that we have terrible diets. We have toxic exposures. We have a lot of adverse childhood events and early trauma for our children. We have a lot of chronic stress as adults, and we don’t have enough hormetic stress followed by sufficient recovery time.
Casey Means: While I feel like it can be overwhelming for people to think of all those things that need to be right—it can almost seem hopeless—I think it’s actually really an opportunity because there are so many different areas that you can focus on to do right by yourselves.
Terry Wahls: What I want people to do is to start small. When I talk about behavior change, I invite them to think about some aspect of their health behaviors that they could begin to improve. We get curious. We’re going to talk about diet. We’re going to talk about meditation, exercise, sleep. In some of my studies, we make you do everything all at once. In some ways, that’s easier. In my clinical practice, that’s going to be a very kind conversation like, “Okay, so here are the domains, where do you want to start? Let’s come up with a goal that you’re confident you can really do. Because I want you to have a change that you can actually do as opposed to a change that you only do 50%. Then we build on that success.”
Casey Means: Such a wise approach—giving people manageable entry points to start seeing that success and then using that as a way to really fuel and catalyze continued behavior change.
Terry Wahls: And just to insist that people do the Wahls diet first. I actually have become a little more mellow about that now, realizing that some have to meditate first and get their stress down to be more manageable, and then they can begin addressing food choices.
On the relationship between metabolic disease and neurodegeneration
Casey Means: You and I had a conversation recently about a really interesting chemical in the body called Osteopontin, which is secreted in the adipose tissue. When it’s high, it can have really negative and toxic effects on the brain. This cytokine is one of these links between metabolic disease, high levels of visceral fat and visceral adiposity, and neurodegeneration and neurologic disease. Can you describe this relationship and what we’ve learned about it?
Terry Wahls: It’s also involved in bone health. It’s an important compound there. We know that it is involved in immune regulation and people who have rheumatoid arthritis, systemic lupus, MS have been seen to have elevated levels of Osteopontin. When I was at one of my MS research meetings, I was listening to researchers talk about Osteopontin’s effect on the microglia. The microglia are the monitors of the brain environment. If the microglia see the brain environment as hostile, they will begin attacking the invaders and killing brain cells and killing myelin and killing synapses, and leading to rapid atrophy of the affected parts of the brain. The microglia can see, “This is a great environment. Everything looks good, but I see a few strained synopses in parts of the brain that need nurturing support. So I’m going to go there, secrete all of these nurturing compounds and I’ll repair the myelin, I’ll repair the synapses.”
Microglia can be restorative or destructive. What intrigued me was that they were discussing how high Osteopontin accelerates the microglia to be very destructive, which then got me into reading. This has been known for some time. This has been reproduced—that Osteopontin can shift the microglia to be more destructive. What drives high Osteopontin? Insulin resistance. Too much central obesity. I have a freezer full of specimens. We’ve been writing grants. We just submitted a grant to look at our freezer, and Osteopontin was one of the biomarkers that we proposed to analyze. The funding cycle will run for three years. It’ll be three years before I’ll know this answer, but hopefully, in three to four years, we can have this conversation and we’ll be able to tell what we saw.
Casey Means: From what it sounds like, if people can improve their insulin resistance, their central obesity, and visceral adiposity, then they might be able to actually reduce levels of Osteopontin, and this could have a downstream positive effect on microglia.
Terry Wahls: Correct. This might be one of the mechanisms [that explain] why high blood sugar accelerates cognitive decline and worsens Alzheimer’s, probably through the microglia. That’s part of the mechanism. It would be my conjecture. We’d have to have some experiments to investigate that, but it certainly seems plausible.
On understanding Type 1 diabetes within The Wahls Protocol framework
Casey Means: Another autoimmune disease that I think is of great interest to the people listening to this podcast is Type 1 diabetes. Mostly we focus on Type 2 diabetes in the spectrum of acquired insulin resistance and the hyperglycemia that comes from that. But of course, there’s this whole other branch. Type 1 diabetes is the autoimmune destruction of our pancreatic beta cells, which reduce our insulin. It’s less an issue of insulin resistance and more an issue of not having enough insulin around. Does this disease state also fit within the Wahls Protocol framework? Is there anything from the framework and what we know about mitochondrial dysfunction and microbiome effects on autoimmune propensity that can be applied to Type 1 diabetes?
Terry Wahls: Yes. When we look at the dramatic uptick of autoimmunity, since World War II, they talk about inflammatory bowel disease, MS, and Type 1 diabetes. There are environmental factors that are tied in, probably the change in the food supply, the dramatic increase of fructose, the dramatic increase of sugar processed foods, the increase of synthetic chemicals in our diet, and the dramatic shift in our microbiome because of all of the antibiotics. All of those factors in why those three autoimmune diseases have increased. It’s not just the infection that triggered the destruction of the pancreatic islet cells. It is the environment that sets that cascade up. I’ll also tell you that we’ve had certainly many, many patients with Type 2 diabetes tell us that they’ve reversed their diabetes using the Wahls Protocol, but I’ve also had many people with Type 1 diabetes tell me that they’ve had dramatic improvement of their blood sugars in their management of their disease using the Wahls Protocol.
There was one lady who has a fairly remarkable story. She had pulmonary sarcoidosis in addition to Type 1 diabetes and was in ICU because of her severe sarcoidosis. She was on a very high dose of prednisone to control her sarcoidosis. While she’s in ICU, one of her neighbors—here’s my very first lecture that I gave here in Iowa City—went to see Julie and her husband to say, “When you get out of the hospital, we’re going to cook for you because I know how life is just so difficult.” The food they cooked was based on the principles that I laid out in that very first lecture, which looks very much like the principles that I teach in my TED Talk. Her sarcoidosis melted away, stunning her physicians. She was able to get off her prednisone, and her insulin control became much, much better. Her renal disease had been very severe. She was on the brink of needing dialysis and her renal function improved remarkably. It was no longer an immediate threat for needing dialysis.
I finally met her about five years after the fact at another conference. She told me that story. Part of why I’m sharing that whole story for you, Dr. Means, is, and of course, I had no idea of the impact that I had for Julie, that you don’t know the ripple effect of these podcasts, nor do I know the ripple effect of that Ted Talk or my books or the practitioners that I teach. But the work we are doing is transforming the lives of millions and millions of people. I so appreciate that you’re taking the time to do these podcasts. I appreciate that you had the brilliant insight to create Levels, to give people the tools, to get their insulin resistance under better control. It will have this ripple effect of millions and millions of lives.
Casey Means: Thank you. And I think that is so powerful. I mean, as I mentioned in the beginning, the ripple effect of your work, even in my own life has been profound. I’m just so grateful to you and many of the authors in this space who have really put themselves out there by challenging the convention and digging deeper and asking the question of why over and over and over again.
On challenging conventional medicine comfortably and respectfully
Terry Wahls: When I first started having these public conversations, let me tell you, the neurology community was very upset and severely condemned over and over again. Fortunately, I stuck with it. I kept doing my little research, getting our papers published, writing our grants. I now have a joint appointment in neurology. My neurology colleagues are coinvestigators on my grants. I just got comments today from the chief of neurology on my current proposal. He’s like, “Oh my gosh, Terry, this is very compelling, very exciting.” And so I’ve come a long way in these 11 years from being condemned as intolerably dangerous to being seen as having these really interesting, innovative ideas that now my very conventional chief of neurology, who is the chief of the MS clinic, thinks are brilliant and visionary.
Casey Means: It takes a lot of bravery to be one of those first voices.
Terry Wahls: When I first started changing how I practiced medicine, people were complaining. My chief of medicine, the chief of staff at the VA called me in, had me explain myself. Then I had to go have the same conversation with the chief of medicine at the university, who said, “Terry, you’re going to lose your license because all we need is somebody to file an anonymous complaint. You’ll get inspected. You’ll be inspected by people who don’t believe in functional medicine, integrative medicine. You need to learn how to talk about this.” They sent me to work with the chief of the complementary alternative medicine clinic. Actually, I was very grateful that they did. It became very clear with my patients and with the public that I’m focused on creating health. We’re going to really focus on modifiable lifestyle factors, and we’ll see what your body can do with that. I’ll have to watch you closely for your blood pressure, your blood sugar, and your current medication use so you don’t become over-medicated, but we’re going to focus on creating health using these basic lifestyle principles.
When I shifted how I spoke to my patients and the residents, I quit getting complaints. When I focused my clinical notes that way, I quit getting complaints. My chief of staff and my chief of medicine said, “Attagirl, we appreciate that you’re doing that. That’ll be fine. You’ll be able to pass peer review because we need you to pass peer review, Terry.” And so that’s my caution when I train practitioners. We have to teach you how to talk about this because you and I get so excited, it’s so clear, like, “Oh, my God, this is treating and reversing so many disease states.” But we have to be very careful that what we are doing is we’re focused on creating health and monitoring current medication use and adjusting them so people aren’t overmedicated. Because that language will feel very comfortable to our conventional colleagues and very respectful.
As soon as I say, “I’m treating MS with diet and lifestyle,” that’s not FDA approved and that can’t be sanctioned and that will not pass peer review. But if I say, “I’m focused on creating health by treating diet and lifestyle, and we’re going to watch your medications and adjust them so your blood pressure doesn’t become too low, your blood sugar doesn’t become too low, and then you can talk with your neurologist about what makes clinical sense to you,” everyone is very happy with that. My neurologist colleagues are happy with that. My chief of medicine is happy with that. My chief of neurology is happy with that. We have to be careful that we teach our functional medicine practitioners how to talk about this in a way that respects conventional medicine, respects the patients, respects the healing process. Because what we’re doing is we’re creating health, and as a side effect, sometimes—not always, but sometimes—you regress a considerable amount of pathology as a side effect of creating health.
On the underlying connection between different autoimmune diseases
Casey Means: Before we conclude, there’s one question that is lingering in my mind that I really want to take an opportunity to ask you. We’ve got all these different autoimmune diseases that look very, very different, from type one diabetes to rheumatoid arthritis to lupus to MS. What you talk about in the book is that there are really just a handful of core physiologic features that have gone awry that can lead to all of these things. How does that happen in the body, wherein one person it might look like lupus, in one person, it might look like rheumatoid arthritis, and in another person, it’s MS.
Terry Wahls: Isn’t that really interesting? We have disordered immune function, we have weakened mitochondria, we have toxin overload, we have hormone imbalance, we have difficulty eliminating our toxins. I have different sets of microbes in my gut. And then I have different genetic vulnerabilities. So, depending on the microbes and my genes, when my immune system gets revved up, and I begin making autoantibodies that will begin clearing out that infectious problem or that food protein that I think is an infection if that protein has a similar amino acid sequence to another structure in my body, in my brain, in my joints, in my lungs, in my skin—that part of my body is going to get damaged as I clear out that problem protein, whether it’s an infection or a food protein.
My vulnerability is a reflection of my genetics, my microbiome, the foods, and the similar amino acid sequence between my structures and those various proteins. I’ll add to that—and we can use myself as a case in point— as a youngster, I have migraines. That’s an early prodrome. I have really heavy periods. A lot of women have miserable, heavy, heavy, heavy periods. When I decided I want to have kids, I discover I have severe, severe endometriosis. [I’m] going through IVF. By then, I’d already had 10 years of my trigeminal neuralgia, which was the autoimmune process involving my brain. I had an autoimmune process involving my brain. I have asthma, an autoimmune process involving my lungs. I have an autoimmune process involving endometriosis. And I have very mild psoriasis.
If you don’t address the root causes, you keep developing more autoantibodies. More autoimmune processes in more parts of your body will become casualties in the autoimmune process development. One of my messages to people is, yeah, you may need disease-modifying drug treatment for your autoimmune disease. But if you don’t address the underlying root causes, you will continue to develop other autoimmune processes through this molecular mimicry. You will pick up another body part casualty, whether it’s asthma or psoriasis or endometriosis, or autoimmune thyroid disease. You want to have healthy aging, a healthy brain, and all that stuff. So, everyone, whatever you got, whatever chronic complex health problems you have, you want to be sure that you’re also doing everything you can step by step with your modifiable lifestyle factors.
On the importance of investigating your own insulin resistance
Casey Means: You touched on something there that I think is also important in this metabolic health blood sugar conversation, which is the concept of warped proteins and that these can be a trigger for the body to fight. Can you touch on the relationship between glucose and warped proteins and glycation, and how hyperglycemia might lead to dysfunction in the body?
Terry Wahls: We would be so far ahead in our healthy aging if we would all check our glucose and check for the possibility of insulin resistance. You can be skinny and have insulin resistance. You can be skinny, not have any central obesity, be thin on the outside, and fat on the inside. If you have elevated blood sugars, you’re going to be at risk for this glycation, the sugar is attached to the proteins, and the proteins become oxidized, nonfunctional, and that will be an accelerant for this autoimmune process. It can be an accelerant for that cell danger response. If you aren’t looking for insulin resistance, you’re going to miss the “thin on the outside, fat on the inside” because we have so deranged our diets, we have had such terrible diets for so long that, I don’t know what the percent would be that actually have insulin resistance, but it is probably far higher than the rate of obesity. I don’t know, because I don’t know that anyone has done any kind of population basis to really look for that number.
Casey Means: I would love to see a big retrospective study looking at a large, hospital system, triglyceride-to-HDL ratio, which is something we already have cholesterol panels on everyone. That would give us at least a hint at insulin sensitivity, which could be really interesting.
Terry Wahls: That’s a good idea. I could mention that in my post.
Casey Means: Every adult patient has that cholesterol panel and it’d be fascinating to see who’s over one of a ratio, who’s over two, who’s over three. Does it correlate with BMI? Does it correlate with blood pressure? This would be fun to work on.
Terry Wahls: That could be a nice epic study for a large dataset, such as women’s health initiatives.
On the best ways to support mitochondrial health
Casey Means: To wrap up, what are some of your top recommendations for what people can do to support their mitochondrial health through diet and lifestyle
Terry Wahls: Number one, ditch all the sugar, sweets, and beverages. Number two, ditch all the fructose, all of those paleo-friendly sugar substitutes that are all fructose Get rid of those. Number three, replace grain-based products with vegetables. Number four, I’m a tall lady, six feet tall. It’s pretty easy for me to have nine cups of vegetables a day: three cups of green, three cups of sulfur, three cups of color. But I don’t know how tall you are.
Casey Means: Six feet.
Terry Wahls: Okay! We can both have our nine cups, no problem. If you’re a meat-eater, 6 to 12 ounces of meat. If you’re not a meat-eater, gluten-free grains, and legumes for your protein.
Casey Means: Perfect. Well, I hope that this conversation is very uplifting for anyone listening who is on the spectrum of autoimmune disease. The key message that we’re talking about, that you’ve promoted in such a beautiful way over the last decade, is that there is so much hope. There is a lot that we can do, but we do have to change the choices that we’re making every day. But these choices can be wonderful, like including more beautiful vegetables, and they work. Would you say that it’s safe to say that focusing on improving metabolic health can be part of a journey in moving towards the improvement of autoimmune disease?
Terry Wahls: Yeah. Let me be even stronger. I think everybody with an autoimmune disease really should go investigate their metabolic health. Know your glucose, your insulin levels, your A1C, and answer the question: do you have developing insulin resistance? If you do, then we need to have a strategy for dealing with that. If you have an autoimmune disease, I very strongly urge you to investigate whether you have insulin resistance.
Casey Means: Thank you so much for taking your time today to educate this audience. I really appreciate you being here, Dr. Wahls.
Terry Wahls: Thank you.