As our primary sense, vision is critical. According to a recent study, most Americans consider loss of eyesight as the worst ailment that could happen to them, surpassing such conditions as loss of limb, loss of memory, loss of hearing or speech, or having H.I.V./AIDS. The consequences of vision loss can be profound. Studies in individuals with visual impairment (low vision and/or blindness) have reported difficulty functioning in daily activities, along with a reduced health-related quality of life and increased rates of depression and anxiety.
“Our eye health is intimately connected to our overall health, especially our metabolic health, though few people know about this connection.”
A common misconception is that all eye problems noticeably affect vision and are thus easy to detect based on visual changes alone. Unfortunately, this is not the case. Most eye problems, especially in their early stages, can exist entirely without symptoms. Because most visual changes progress slowly and gradually over time, it is unlikely that an individual themselves would detect a change in vision until the condition is much more advanced. In one study, approximately 1 out of 4 people presenting to an eye exam for refractive complaints only (i.e., seeking a prescription for glasses or contact lenses because of blurred vision) were also incidentally found to have some form of ocular pathology. This is a testament to the frequent existence of ocular conditions that go undetected without the intervention of an eye care provider, as well as the importance of a regular eye exam.
An eye exam not only detects undiagnosed eye conditions but sometimes even undiagnosed systemic health conditions. Our eye health is intimately connected to our overall health, especially our metabolic health, though few people know about this connection. Even among people with diabetes, 40% to 45% have had diabetes affect their eyes, but only about half are aware of it, according to the National Eye Institute. In one study, only half of the people with diabetes knew that diabetes could cause eye problems and that dilated eye exams are important; the same study found that only a third knew that strict diabetes control could prevent eye problems.
Eye exams are important not only for the diabetic population but also for the general population, especially as a spectrum of metabolic conditions is rising. As of 2018, only 12% of Americans are metabolically healthy, meaning a vast majority (88%!) of Americans are metabolically unhealthy and could affect their eye health.
This article explores how metabolic health and blood glucose levels can affect almost every aspect of the eye, literally from front to back, and how metabolic control and awareness through metabolic fitness and continuous glucose monitoring may be beneficial for the proactive maintenance of your metabolic and eye health.
Let’s start at the front of the eye and work backward.
1. Increased risk of dry eye disease
Dry eye is a disease of the ocular surface that occurs due to tear film abnormalities, either in quantity or quality of the tears, causing dryness, irritation, and eventually damage to the eye’s front surface (the cornea). Dry eye disease is typically due to multiple factors, including poor diet, poor systemic health, poor lid hygiene, inadequate blinking, and/or inadequate production of one or more components of the tear film.
The consequences of dry eye disease span further than just mild discomfort. Dry eye disease can significantly affect vision due to an increased risk of painful corneal ulcers, infection, scarring, irreversible corneal damage, and vision loss. Additionally, patients with dry eye disease are sometimes in chronic pain with burdensome or ineffective treatments.
Although there are currently no studies regarding dry eye and blood sugar levels in non-diabetic individuals, dry eye has a known association with diabetes, especially in those with poor glucose control. Studies in diabetic individuals have shown that those with higher glucose levels and poorer glucose control (measured via HbA1c) are at a higher risk for dry eye and are more likely to lose the oil glands in the eyelids that are critical for tear production and stabilization.
Similarly, another study found that diabetic individuals showed decreased tear production, decreased corneal sensitivity, and decreased tear stability, especially in individuals with peripheral neuropathy and poor metabolic control.
Bottom line: Metabolic health and strict control of glucose levels could play a role in producing healthy tears and maintaining the health of the front of the eye.
2. Increased risk of developing cataracts
A cataract is the clouding of the lens inside the eye. This lens is aptly named the intraocular lens and is located behind the front of your eye (the cornea) and the colored part of your eye (the iris). Its job is to bend the light that enters the eye to focus it on the back of the eye (the retina). The retina is the neural tissue in the back of the eye that captures light and sends signals to the brain, which are then interpreted and perceived as vision. This process and the act of focusing light on the retina is key for creating clear sight.
At birth, the intraocular lens is clear and inevitably will slowly become more opaque or cloudy over time due to the natural processes of aging. With a cataract, the lens is no longer clear, and the light is not bent as cleanly; instead, it scatters in many directions. Without a clear focus on the retina, this translates to blurry and cloudy vision that could require cataract removal.
Our metabolic health and blood sugar levels can affect the intraocular lens. One condition that has been correlated with cataract is metabolic syndrome. Metabolic syndrome is a combination of multiple components that indicate poor metabolic health, including high blood sugar, high blood pressure, abnormal cholesterol levels, and obesity.
In a study involving individuals with metabolic syndrome, the prevalence of cataract increased with an increasing number of metabolic syndrome components. Additionally, individual components of metabolic syndrome (diabetes and high blood pressure) were individually associated with cataracts, even after adjusting for age, sex, smoking status, and education. (A caveat here is that this is correlation and not causation; however, this is good evidence.)
This study also found:
- The combination of diabetes, high blood pressure, obesity, and low high-density lipid levels = 7x odds of having cataract
- The combination of diabetes and high blood pressure = 4x odds of having cataract
In another study, individuals with metabolic syndrome were also shown to have an increased risk of needing cataract-removal surgery.
Another condition that is correlated with cataracts is diabetes. In one study, people with diabetes were found to have 2-5x more risk of cataract formation and were more likely to get cataracts at a younger age. Recovery after cataract surgery for diabetics can also be more complicated with fluctuations in blood glucose levels.
Bottom line: Factors of metabolic health including weight, blood sugar, blood pressure, and cholesterol levels can increase the risk of developing a cataract. High blood sugar levels could cause earlier cataracts and possible complications in cataract surgery.
3. Temporary fluctuations in vision due to blood sugar levels
Staying within the intraocular lens topic, high blood sugar levels are thought to cause transient thickening or swelling of the lens, causing temporary fluctuations in vision.
It is well known that high blood glucose levels can cause temporary near-sightedness in people with diabetes. In one study with non-diabetic subjects, an increase in plasma glucose was induced along with a pharmacologically induced insulin resistance to mimic a diabetic state of hyperglycemia. The induced 400% increase in blood glucose levels resulted in a myopic (nearsighted) shift of 2 diopters, which reversed when blood glucose returned to normal. “Diopters” likely means nothing to the average reader, but think of them as the unit used to measure nearsightedness or farsightedness in a glasses prescription. Below is a visual representation of the magnitude of 2 diopters of nearsightedness (on the right) when compared to clear 20/20 vision (on the left). This demonstrates the visual impact very high blood glucose levels can have on sight.
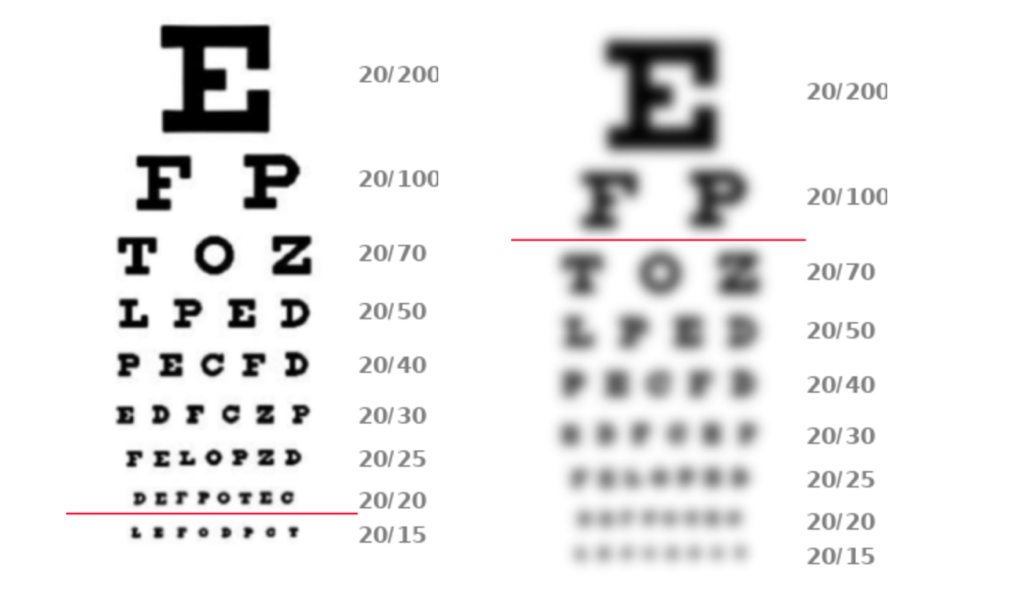
Bottom line: Blood glucose levels could affect the prescription in your glasses/contact lenses, causing fluctuations in vision.
Now, let’s explore the effects of metabolic health on the back of the eye, the retina.
4. Changes to the retinal microvasculature and circulation
As previously stated, the retina is the neural tissue (yes, our eyes are part of our brain!) in the back of the eye that converts light into electrical signals, which are then sent to the brain via the optic nerve to create the perception of vision. Retinal health is critical, and without a properly functioning retina to translate light into vision, blindness occurs.
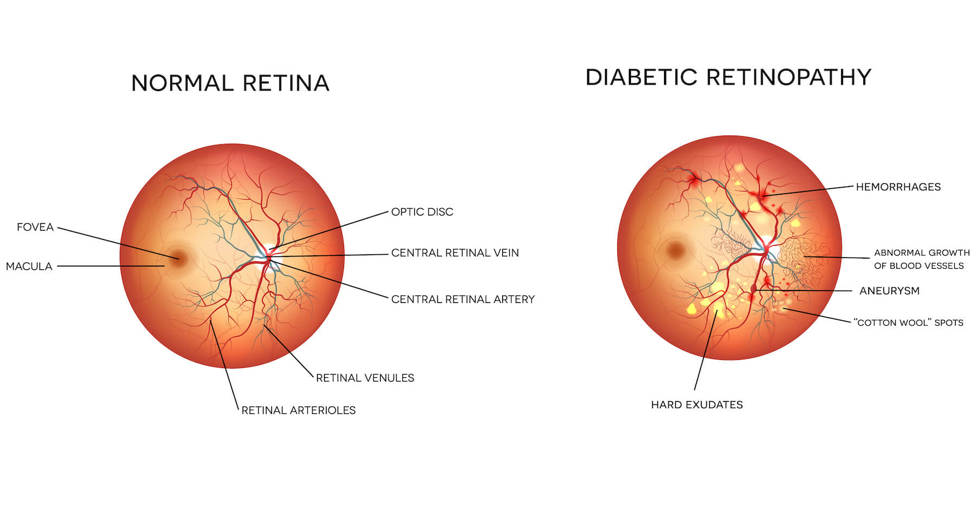
A dilated retinal exam is the only time a physician can directly observe blood vessels in the body in vivo and without an incision, making it an excellent, non-invasive method of examining ocular and systemic metabolic and vascular health (pretty cool, right?). The retina has its own circulatory system to supply and remove blood and nutrients, consisting of microvasculature such as the retinal venules, arterioles, and capillaries. Subtle retinal microvascular changes in these vessels (i.e., retinal microaneurysms, arteriovenous nicking, focal arteriolar narrowing) can indicate a problem with microvascular health, not only in the retina but all over the body.
Metabolic syndrome has been associated with large and small vessel inflammation and damage, and there is evidence that metabolic health can affect the retinal microvasculature. In one study, advanced imaging of the retinal microvascular circulation found altered blood flow present in individuals with impaired glucose tolerance prior to the development of diabetes or cardiovascular disease.
In another study, individuals with metabolic syndrome were more likely to have retinopathy and retinal microvascular changes than people without metabolic syndrome, independent of age, gender, race, education, smoking, or alcohol consumption. Associations with retinal microvascular changes were significant even in people with metabolic syndrome without diabetes and high blood pressure.
Bottom line: This is good evidence that optimizing blood sugar levels and metabolic health (including blood pressure, weight, and cholesterol) could help maintain proper circulation within the small vessels of your eye and the rest of your body.
5. Increased risk of retinopathy (retinal disease)
Beyond subtle microvascular changes in the retina, systemic metabolic and vascular disease can lead to progression to frank retinopathy (retinal disease) with retinal hemorrhages (bleeding in the back of the eye) and signs of retinal ischemia (tissue death due to inadequate blood and oxygen supply).
The process of retinopathy begins with microvascular abnormalities that lead to reduced blood flow to the retina. The oxygen-starved retina then sends signals that start constructing new blood vessels to try and bring more blood (and thus more oxygen). However, these blood vessels are built rapidly and shoddily, meaning they are more fragile and prone to break and leak. After a bleed, the risk is not over. Blood is reabsorbed but leaves fibrotic material (scar tissue) that can pull on the retina and lead to a retinal detachment and subsequent blindness.
Blood sugar levels have been correlated with retinopathy in several studies. In people with diabetes, strict control of blood sugar reduced the risk of retinopathy and the need for ocular surgery by 76% in type 1 and 21% in type 2 diabetes. Blood sugar levels were also important for non-diabetics. One study in non-diabetic individuals found that increased blood sugar levels (measured via HbA1c) and waist to hip ratio were correlated with retinopathy. In this same study, retinopathy was found in 7.3%, 13.6%, and 17.5% of individuals with normal, impaired, and diabetic glucose metabolism, respectively, suggesting those with better glucose control had less chance of having retinopathy.
The above studies are significant as evidence that individuals have control over their retinal health via control and optimization of blood glucose levels.
Beyond glucose levels, overall metabolic health is important for preventing retinopathy as well. For instance, high blood pressure is the best known systemic condition associated with non-diabetic retinopathy, and poor blood pressure control is tied with worsening microvascular damage. An independent association between retinopathy and other metabolic health factors, such as high blood pressure and larger waist circumference, has been found.
In a study with diabetic individuals, those with tight blood pressure control had a 34% reduction in progression of retinopathy, a 47% reduced risk of deterioration in vision, and a reduced risk of stroke and death.
Studies in diabetic individuals also found that the more factors of metabolic syndrome an individual had, the more likely they were to have diabetic retinopathy. In contrast, tight metabolic control significantly decreased diabetic retinopathy and major cardiovascular events and increased quality of life.
Bottom line: Optimizing blood glucose levels, both in diabetic and non-diabetic individuals, could reduce the risk of retinopathy/retinal disease.
6. Increased risk of retinal vascular occlusions (aka increased risk of stroke in the eye)
Beyond the microvascular implications concerning the retinal arterioles and venules, permanent, significant, and sudden vision loss can occur due to large vessel involvement in the retina via occlusion of the retinal arteries or veins. This essentially constitutes a stroke in the eye and could mean that a systemic stroke is impending.
Metabolic health can be connected with vascular occlusive events. Diabetes and high blood pressure, in particular, are known to be associated with vascular damage and an increased risk of large vessel atherosclerosis. Central retinal artery occlusion has a known association with high blood pressure and diabetes. Additionally, high blood pressure and obesity are significant risk factors for central retinal vein occlusion.
In a study in non-diabetic individuals with a history of retinal vein occlusion, 53% of individuals had abnormal results on a glucose tolerance test, along with reduced retinal arterial blood flow. Notably, this indicates that poor glucose metabolism, even without diabetes, may be correlated with retinal vein occlusions.
Bottom line: Controlling metabolic health can reduce your risk of a vascular occlusive event (a stroke) in the eye. Some evidence suggests that impaired glucose metabolism could be associated with these occlusive events.
7. Increased risk of macular disease
One area of the retina is crucial as it is responsible for our clearest, central vision. (In fact, you’re using it right now to read this article.) This is the area known as the macula. When the macula is damaged, this interferes with the central vision that we rely upon in our daily lives to function.
In people with diabetes, swelling and leaking fluid in the macula (known as macular edema) can cause irreversible vision loss. In a meta-analysis, some studies suggested that significantly elevated triglycerides, low-density lipids, and total cholesterol were correlated with diabetic macular edema, suggesting again an intersection between poor metabolic control and diabetic changes in the eye. However, this remains to be further examined.
Additionally, one study found a higher risk of age-related macular degeneration in individuals with high blood pressure or higher BMI.
Bottom line: Metabolic health, including glucose metabolism, BMI, and cholesterol levels, could impact the part of your eye that is responsible for your clearest, central vision.
8. Increased risk of increased eye pressure and glaucoma
Glaucoma is a condition that affects the nerve fibers of the eyes and their pathway of communication with the brain, known as the optic nerve. Damage to the optic nerve causes irreversible vision loss. The full mechanism of glaucoma is not yet fully understood; however, it has been shown that elevated pressure in the eyes, known as intraocular pressure (IOP), is associated with glaucoma progression. One theory is that elevated IOP could cause microvascular damage around the optic nerve causing chronic nerve damage and eventual nerve death. The only known effective treatment for glaucoma is lowering intraocular pressure, which has been shown to slow disease progression.
There is some evidence that supports an association between elevated IOP and metabolic syndrome. One study found an association between IOP and BMI. Another study found an increase in IOP in subjects with metabolic syndrome compared to those without and an increase in IOP with increasing components of metabolic syndrome.
However, having elevated IOP does not automatically mean you have glaucoma, as glaucoma is defined by structural and visual changes, not by eye pressure alone. A recent review of the literature on metabolic syndrome and glaucoma as of 2020 highlights a lack of prospective studies in patients. However, the only prospective study that has been conducted found that patients with higher BMI or more components of metabolic syndrome were more likely to develop open-angle glaucoma.
Additionally, in diabetics, a unique form of glaucoma can occur due to the growth of new blood vessels in the eye’s drainage system. These blood vessels back up fluid in the eye leading to a subsequent increase in eye pressure. This form of glaucoma is known as neovascular glaucoma, and its incidence increases with duration of diabetes and poor blood sugar control.
Bottom Line: High blood glucose levels and poor metabolic health may be associated with increased eye pressure that could result in glaucoma.
Wrap up
Evidence suggests that metabolic health and blood glucose control could be key in maintaining eye health, especially in those with metabolic syndrome and diabetes, and in those without either diagnosis. Continuous glucose monitoring and the ability to make educated decisions regarding our metabolic health promote better overall health and eye health.
A brief soapbox moment and to end on a positive note – It’s not all doom and gloom! The good news is that many of the above-mentioned conditions are easily diagnosed in a dilated eye exam, and effective treatments do exist. Sacrifice one afternoon of blurry vision (also known as a dilated eye exam) once a year to have your eye care professional evaluate your eye health — even if you think you don’t need it! Remember, early detection is key, and early treatment is oftentimes extremely effective in slowing or stopping disease progression. Don’t wait until you have vision problems to see your eye doctor. Plus, we’re nice people, so come meet us!
About the Author

Dr. Kellen Riccobono is a fellowship-trained optometrist and a Fellow of the American Academy of Optometry. She completed her undergraduate coursework with honors at the University of Texas at Austin. Afterward, she received her Doctor of Optometry degree from The University of Houston College of Optometry, graduating summa cum laude. Dr. Riccobono completed a post-graduate fellowship at the same institution, specializing in corneal disease and medically necessary contact lenses. During her fellowship, Dr. Riccobono developed an interest in both writing and clinical research. She has experience in medical writing, ranging from research protocols to articles in Review of Optometry and co-authoring publications in journals such as the American Journal of Ophthalmology & Contact Lens and Anterior Eye. Kellen is passionate about medical optometry and believes in the importance of providing compassionate and comprehensive care to her patients and spreading awareness of the importance of ocular health.