Additional medical review by Dr. Javier Diaz, Pharm D., FAARM, FMNM, ABAAHP, RPh, METS; Dr. Richard Harris M.D., Pharm D., MBA; Jordan Mazur MS, RD; Dr. Daniel Wallerstorfer, PhD; all of Rootine.
Carbohydrates, protein, and fat dominate the metabolic fitness discussion. While these macronutrients are critically influential in how our body produces energy and wards off disease, they certainly don’t act alone.
We also need micronutrients. These include vitamins, minerals, trace metals, and antioxidants that together play a synergistic role in maintaining a healthy immune system and keeping your body running optimally at the cellular level. Micronutrients are like the tools that assist your cells in carrying out their usual functions.
“Despite relatively nutrient-rich soil, as much as half of all Americans are deficient in at least some micronutrients.”
Most are crucial links in chain reactions that involve proteins, enzymes, and hormones that regulate every part of your body’s metabolism. If one of the links is weak or missing, the entire system malfunctions. They can act as activators of critical chemical reactions, building blocks of key proteins, and more.
Research connects micronutrient deficiencies—especially calcium, magnesium, and zinc—to insulin resistance and shows that conditions like obesity and Type 2 diabetes can affect micronutrient levels.
Some micronutrients are easier to come by than others, and the nutritional content of your food can vary greatly depending on where it’s grown and what kind of nutrients are in the soil. But despite relatively nutrient-rich soil, as much as half of all Americans are deficient in at least some micronutrients. Here are the eight most essential micronutrients for metabolic fitness, what they do in the body, and how to make sure you’re getting enough.
Note that all micronutrients play multiple roles in your body; here, we’re focusing specifically on the metabolic functions of these nutrients. Individual micronutrient needs can also vary depending on genetics and lifestyle. Talk to your doctor about how much of each micronutrient you should be aiming for.
The Micronutrients
Vitamin D
Magnesium
Selenium
Zinc
Omega-3 fatty acids
Vitamin B (B12, B6, folate)
Lipoic acid (alpha lipoic acid)
Manganese
Vitamin D
Promotes bone health, aids glucose, insulin control, and immune function

Metabolic Role: When it’s eaten or produced from sun exposure, your liver metabolizes vitamin D before enzymes in the kidneys turn it into its active form, a metabolite called calcitriol. The vitamin is usually best recognized for its role in bone health. That’s because calcitriol regulates calcium and phosphate metabolism, the primary minerals that strengthen bones, and how the skeleton can utilize the nutrients.
Research shows associations between low vitamin D levels and obesity, insulin resistance, and heart disease (especially hypertension), and low vitamin D is common in people with Type 1 and Type 2 diabetes. Proposed mechanisms for why vitamin D affects insulin include its anti-inflammatory effects, including around pancreatic cells that produce insulin (the immune cells that cause inflammation have vitamin D receptors, and vitamin D seems to inhibit their response); and its effect on calcium, necessary to release insulin.
A 2018 meta-analysis found significant effects of vitamin D supplementation on several groups, particularly people with prediabetes. For example, vitamin D significantly lowered fasting glucose in people with BMI less than 25, people with prediabetes, and people with vitamin D insufficiency. The study also showed decreased incidence of Type 2 diabetes after vitamin D supplementation without calcium, in overweight people, and in people with prediabetes. Other studies have shown similar metabolic effects from vitamin D in the elderly and in obese adolescents.
How Much Do You Need: Adults younger than 70 should get at least 15 micrograms (600 IU) of vitamin D daily, while those over 70 should aim for closer to 20 micrograms (800 IU). Some studies use much higher doses. For instance, in a study showing a reduction in fasting glucose with prediabetes, the dose was >2,000 IU per day. Blood concentrations should be >20 ng/mL based on standard criteria, although some physicians recommend higher levels in the range of 40-60 ng/mL.
How to Get It: It’s not called the sunshine vitamin for nothing––50 to 90% of vitamin D intake comes from sun exposure. But how much time you need to spend in the sun to get the correct dose of vitamin D depends on a lot of factors, including where you are on Earth, the time of year, time of day, how overcast the day is, and your complexion. But Vitamin D3, one of the two primary forms of the vitamin, can either be produced when sunlight hits the skin or absorbed from eating meat or in supplement form, so you have options. Vitamin D2, the other major form of vitamin D, mainly comes in the form of a manufactured additive (created by exposing a kind of mold to UV light) that’s added to foods or taken as a supplement. Some studies show certain vitamin D is absorbed better when eaten with higher-fat foods.
Three ounces of trout or salmon will get you near the recommended amount, and half a cup of mushrooms grown with UV light contain almost half of the vitamin D you need in a day. If you’re worried that you aren’t getting enough through your regular diet, one tablespoon of cod liver oil contains over 200% of the recommended daily dose.
Magnesium
Improves insulin sensitivity and glucose processing, may reduce inflammation
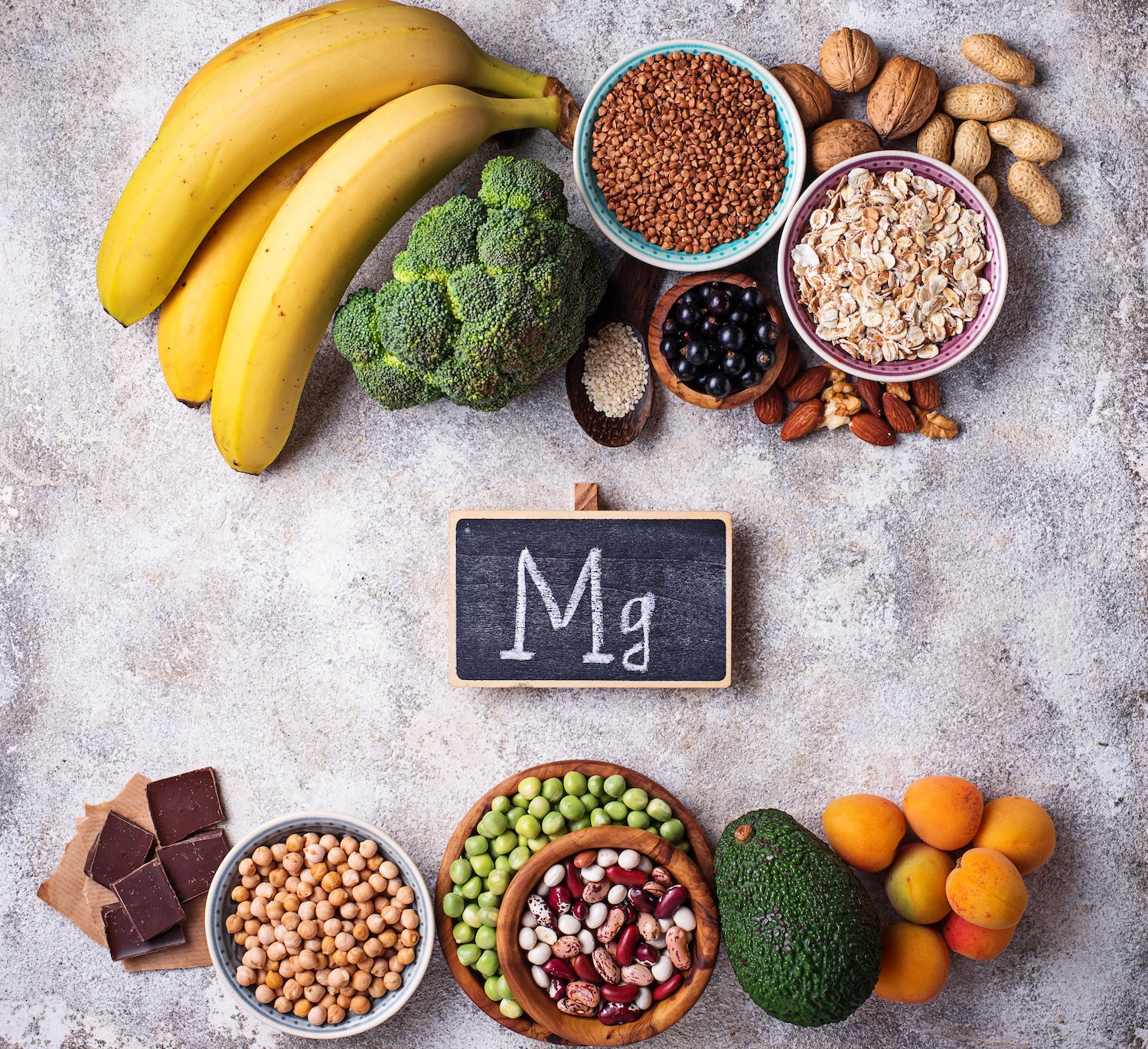
Metabolic Role: Vitamin D doesn’t act alone. The enzymes that metabolize vitamin D require magnesium to function. A meta-analysis that included six studies and nearly 25,000 people found a significant relationship between metabolic syndrome and magnesium deficiency. The researchers determined that for every daily increase of 100mg of magnesium per day, a person’s overall risk of having metabolic syndrome decreased by 17%.
Magnesium is the second-most-abundant positively charged ion in our cells, so there are several proposed ways that it affects glucose metabolism and insulin sensitivity. First, magnesium promotes a biochemical process called autophosphorylation, in which it allows phosphorus to bind to an insulin receptor and switch on the receptor, which aids insulin sensitivity. The mineral also plays a role in enabling glucose transporter proteins (like GLUT4) to transport glucose across cell membranes so that cells can absorb and use it. In addition, animal studies have shown that magnesium deficiency may contribute to insulin resistance in ways not related to glucose transport into cells.
Magnesium is also associated with lower levels of low-grade inflammation, which can be a factor in heart disease, high blood pressure, and diabetes. It may prevent inflammatory mediators from being activated.
Finally, magnesium plays a crucial role in glycolysis, the process by which cells produce energy (adenosine triphosphate, ATP) from glucose. It acts as a cofactor, or assistant, for several key enzymes.
How Much Do You Need: Overall, men should aim to get around 400 milligrams of magnesium every day, while women (who aren’t pregnant) should get about 310 milligrams. As many as half of Americans may not be getting the recommended amount of magnesium regularly.
How to Get it: One of the best food sources of magnesium is pumpkin seeds––a one-ounce serving packs in 156 milligrams. An ounce of chia seeds provides 95 milligrams, and almonds, spinach, cashews, and peanuts are also good sources of magnesium. You can also get it from soy milk, black beans, edamame, and peanut butter.
If you get it through supplements, keep in mind that magnesium aspartate, magnesium citrate, magnesium lactate, and magnesium chloride are the forms most easily absorbed by the body in supplement form. Also, remember that taking magnesium supplements can interfere with antibiotics and some medications used to treat osteoporosis.
Selenium
A powerful antioxidant that promotes glucose absorption without insulin

Metabolic Role: The small intestine absorbs selenium that is incorporated into proteins in tissues throughout the body. The trace mineral plays a critical role in metabolic function in several ways: it’s a powerful antioxidant, it can mimic insulin to promote cellular glucose absorption, and it supports a healthy thyroid, which plays a significant role in cellular metabolism. Selenium also helps support glutathione, a key antioxidant.
Selenium’s antioxidant function happens in part through proteins called selenoproteins. These proteins help reduce the production of reactive oxygen species, which can impair function in the pancreatic cells responsible for insulin production and signaling. That oxidative stress can eventually lead to insulin resistance and other metabolic disorders. By reducing this oxidative stress, selenoproteins help maintain healthy insulin levels. Selenoproteins also help increase insulin sensitivity in other tissues like muscle and fat.
In addition, selenium acts as an insulin-mimetic, meaning it can influence some of the same metabolic processes as insulin, like facilitating glucose uptake in cells and glucose production in the liver. Being able to clear glucose while decreasing the need for insulin is potentially helpful, as having too much insulin can eventually lead to insulin resistance. Selenium helps regulate enzymes that control insulin signaling and lipogenic enzymes—which convert glucose to triglycerides—and the liver’s ability to metabolize carbohydrates.
Finally, selenium plays a significant role in the function of the thyroid, which has the highest concentration of selenium in the body. The thyroid produces hormones, commonly known as T3 and T4, that help regulate cellular metabolism, or how your cells create energy. Your body uses these hormones to maintain a healthy weight, body temperature, muscle strength, and nervous system. Enzymes called iodothyronine deiodinases, which convert T4 to its active form, T3, require selenium to function.
How Much Do You Need: Your body only needs trace amounts of selenium—adults should get about 55 micrograms (mcg) a day. However, research has shown that consuming larger amounts of selenium promotes the production of antioxidant selenoproteins. One 2017 literature review found that 200 mcg per day is optimal for preventing or treating thyroid issues. (Note that some animal models show that too much selenium can lead to metabolic disorders, and excess selenium intake can cause problems with nervous system function, hair loss, and, strangely, garlic breath—so don’t go overboard with supplementation. The NIH suggests 400 mcg as a tolerable upper limit in adults, so best to stay below that upper limit.)
How to Get it: The amount of the mineral in a person’s diet is largely tied to where they live and how much selenium is in the soil in which their food is grown. The soil in the United States, Canada, and Japan typically has a lot of selenium, so deficiency is very uncommon in these countries. But food grown in parts of China and Eastern Europe typically doesn’t have much selenium since the soil there contains very little. As many as 1 billion people worldwide may have selenium deficiency.
The best food source of selenium is Brazil nuts. In fact, they contain so much of the nutrient (68–91 micrograms in a single nut) that regularly eating too many can put you at risk for selenium toxicity. Three ounces of yellowfin tuna, halibut, shrimp, sardines, ham, turkey, and steak are also excellent sources of selenium.
Zinc
Crucial for your body’s insulin system

Metabolic Role: The body uses zinc in more than 300 processes. Zinc is essential for many enzymes in charge of synthesizing carbohydrates, fats, proteins, insulin signaling, and vitamin D activation. It plays a key role in supporting the immune system. Unbalanced zinc levels in the body are associated with diabetes and insulin resistance. Specifically, a zinc deficiency may put people at higher risk for obesity and diabetes.
Zinc’s role in diabetes and insulin regulation is complex. Type 2 diabetes results from ongoing insulin resistance and dysfunctional pancreatic beta cells, which release insulin for the entire body to use. And compared to many other types of cells, pancreatic beta cells contain an abnormally large amount of zinc. Zinc is vital for the body’s creation and use of insulin: insulin is usually stored in units of six arranged around two zinc molecules. This structural association with zinc seems to increase the duration of action of insulin and also allows for storage of insulin. It also works with other micronutrients to activate insulin receptors, necessary for insulin to perform its actions.
A meta-analysis that included 36 studies found that zinc supplementation significantly reduced fasting glucose in both participants with Type 2 diabetes and those with high risk who hadn’t developed diabetes. The researchers determined that a few mechanisms were at play. Firstly, people who had higher levels of zinc also had lower levels of glycated hemoglobin, the result of excess glucose “sticking” to blood cells. Zinc also significantly reduced the amount of circulating C-reactive protein, which indicates inflammation, a factor in metabolic disease. Other research has discovered that zinc also reduces the production of proteins called cytokines, especially the inflammatory sort that can contribute to diabetes and diabetic complications. Zinc also acts as an anti-inflammatory by triggering molecules that can reduce and neutralize free radicals, which directly prevents diabetes.
The enzymes that regulate thyroid function also need zinc to do their job. This means that too little zinc can cause an underactive thyroid (hypothyroidism) that doesn’t produce enough hormones. Thyroid hormone deficiency has most closely been linked to heart disease, weight gain, muscle weakness, and high LDL cholesterol levels.
How Much Do You Need: Adult men should get about 11 milligrams of zinc daily while women should aim for 8 milligrams.
How to Get It: The human body doesn’t store zinc, so it’s important to consume it. Three ounces of oysters provide almost seven times that amount. An equal amount of beef or crab has about half the daily recommended amount of zinc for men and nearly a full daily serving for women. If you’re a vegetarian, an ounce of pumpkin seeds or cashews can provide about 15-20% of your daily intake. Just keep in mind that phytic acid, a form of phosphorus found in some seeds, nuts, legumes, and whole grains, binds to zinc and impairs absorption. This makes plant-based foods less abundant sources of zinc than animal foods; however, simple methods like soaking, fermenting, or sprouting foods can significantly reduce phytic acid content. If you take a supplement, consider one that contains copper since excess zinc inhibits copper absorption.
Omega-3 fatty acids
Builds your cells’ structure, reduces inflammation and insulin resistance

Metabolic Role: Humans usually eat at least 20 different types of fatty acids. These fats and oils fall into three categories: saturated, monounsaturated, and polyunsaturated fatty acids. Omega-3 fatty acids are polyunsaturated and have been long documented as the type of “good fat” that lowers LDL cholesterol and is anti-inflammatory. In animal studies, n-3 long-chain polyunsaturated fatty acids (n-3 LC-PUFA)—a kind of omega-3—have been shown to have a protective effect against insulin resistance brought on by a high-fat diet.
That’s because omega-3 fatty acids block the changes to insulin signaling that a high-fat diet causes. This includes keeping stable expression of a glucose transporter protein called GLUT4 in the muscles and the fat. When it’s able to function correctly, GLUT4 reduces blood glucose levels by bringing glucose into cells.
Omega-3s are also the building blocks of cells. When you consume the fatty acids, they are incorporated into the cell membranes of every tissue in the body, where they can later be released under certain stimuli to help moderate biological functions like inflammation.
Omega-3s are recognized for their anti-inflammatory effect. Enzymes convert two types of long-chain omega-3 fatty acids––eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)––into molecules called oxylipins, which help regulate inflammatory response to cell damage. EPA and DHA slow plaque build-up in your blood vessels by lowering the number of inflammatory signaling molecules called cytokines as well as molecules that make it easier for inflammatory cells to stick to arterial walls. They also reduce the number of triglyceride fat molecules your body produces––which lowers heart disease risk––and prevents fat from accumulating in the liver. Omega-3s can also act inside the cell to change gene expression, including pro-inflammatory pathways like NF-kB, and reduce the number of pro-inflammatory cytokines made by the cell.
Some omega-3 fatty acids (along with omega-6 fatty acids) may also convert into prostaglandins, a subset of oxylipins that are short-lived chemicals that are similar to hormones and that regulate cellular activity. But since omega-3 fatty acids and omega-6 fatty acids use the same enzymes, having more omega-3 fatty acids in the body blocks these enzymes’ ability to convert omega-6 fatty acids into inflammatory prostaglandins. Instead, more omega-3 fatty acids are converted into anti-inflammatory prostaglandins.
How Much Do You Need: Your body needs omega-3 fatty acids and their cousins, omega-6 fatty acids. But the typical American diet is high in omega-6 fatty acids—found in refined seed oils, grains, and grain-fed meat—but deficient in omega-3 fatty acids. Men should eat about 1.6 grams of omega-3 fatty acids daily, and women should get about 1.1 grams. However, these standards are only set for alpha-linolenic acid sources, which are upstream of EPA/DHA in the omega-3 pathway, and must be converted through multiple steps to EPA/DHA.
Unfortunately, there is no standardized guideline for daily EPA/DHA intake, but experts recommend at least 250 mg of combined DHA/EPA, with an upper limit of 2-3 g per day. Pregnant and lactating women likely need additional DHA to support brain development of the child.
How to Get It: One tablespoon of flaxseed or flaxseed oil or 1 ounce of chia seeds or walnuts all contain more than enough alpha-linolenic acid for the day. Three ounces of salmon, mackerel, sardines, rainbow trout, or herring are good sources of both DHA and EPA. You can also get your daily dose from supplements, which usually contain fish oil.
Vitamin B (B12, B6, folate)
Aids glucose metabolism, helps produce new cells

Metabolic Role: There are eight B vitamins, often known by their more common names, like thiamine (B1), riboflavin (B2), and folate (B9). All play a role in metabolism, including converting complex carbohydrates to glucose and allowing the body to use fat and protein. Vitamin B6 alone is involved in 150 reactions that regulate glucose, lipid and amino acid metabolism, DNA synthesis, and neurotransmitter synthesis. In addition, epidemiological evidence suggests that higher levels of B6 and B2 may reduce the risk of Type 2 diabetes.
Research also shows multiple connections between vitamin B6 and diabetes. Diabetes seems to both lower B6 levels, and B6 deficiency may contribute to diabetes formation, primarily through one of its components PLP, which affects multiple enzymes around inflammation, immune cells, and amino acids like tryptophan.
B6 also acts as an antioxidant and can help counteract advanced glycation end products (AGEs). Glycation happens when excess glucose molecules attach to proteins and blood cells. AGEs may play a role in diabetes through inflammation and vascular damage; AGEs can also cause and be caused by oxidative stress. B6, in particular PLP, appears to impair AGE formation. A study in rats with induced diabetes showed that B6 supplementation decreased blood glucose levels and reduced oxidative stress and associated cellular damage, particularly in the kidneys.
Other essential B vitamin functions include:
- Improved lipid (fat) metabolism. One study in rats found that five B vitamins, including B1, B2, and niacin, increased metabolic enzyme activity, which decreased the rats’ weight gain, and led to lower lipid levels than a control group on a high-fat diet without B vitamin supplementation.
- Folate (vitamin B9) aids the body in producing healthy new cells and metabolizing amino acids. You also need it to produce DNA and RNA––the genetic material used to make new cells.
- Vitamin B12 and folate help produce healthy red blood cells. If it isn’t getting enough, red blood cells may not develop normally, which can cause a type of B vitamin anemia called megaloblastic anemia.
How Much Do You Need: It varies by form. For B6, men and women over 50 should get 1.7 milligrams and 1.5 milligrams, respectively. Adults younger than 50 should get 1.3 milligrams. For folate, it’s about 400 mcg for adults. All healthy adults should get about 2.4 mcg of vitamin B12 daily. Since B vitamins are not generally stored in the body, it’s important to get them from your diet.
How to Get it: There’s no one-stop shop for vitamins B6, B12, or folate, and some are easier to come by than others.
Folic acid is the synthetic version of vitamin B9, or folate, used in supplements or fortifying food. Folate, on the other hand, occurs naturally in some foods. For example, half a cup of spinach will provide about one-third of the recommended daily amount of folate. Half a cup of black-eyed peas provides about one-fourth of your daily folate, and 3 ounces of beef liver will give you more than half. Asparagus and Brussels sprouts are also good sources.
About 75% of vitamin B6 in food is bioavailable. One cup of chickpeas has about 65% of your daily vitamin B6 needs, and 3 ounces of yellowfin tuna counts for more than half. Three ounces of salmon is about 35%.
According to the National Institutes of Health (NIH), people over 50 should get most of their vitamin B12 from supplements. Adults this age commonly do not have enough hydrochloric acid in their stomach to absorb vitamin B12 from food.
If you get B12 from food, one 3-ounce serving of clams provides more than 3,500% of the daily recommended amount of vitamin B12. Three ounces of wild trout contains about 225% (about 150% for farmed trout), and the same amount of salmon packs in 200%. Three ounces of canned tuna will give you just over the full recommended amount, and one egg is good for about 25%.
Lipoic acid (alpha lipoic acid)
Helps the cells produce energy

Metabolic Role: Alpha-lipoic acid (ALA), also known as lipoic acid or α-lipoic acid, regulates multiple enzymes that control mitochondrial metabolism. The mitochondria are the part of a cell that produces ATP, cells’ energy source. It’s also a powerful antioxidant that can reduce free radicals from several sources. (Although they sound similar, it’s an entirely different nutrient than alpha-Linolenic acid, the omega-3.) Because of that antioxidant capability, it has been studied as a treatment for nerve pain (neuropathy) associated with diabetes.
ALA also stimulates glucose uptake in fat and muscle cell lines. One meta-analysis that included 24 studies found that ALA supplements may lower blood glucose levels in people with metabolic disease, both through decreasing insulin resistance in muscle tissue (and therefore improving glucose uptake in the muscle) by preserving beta cells, which secrete insulin.
How Much Do You Need: There’s no standardized recommended amount, but studies have shown that 300 mg–1200 mg daily can be effective in specific clinical scenarios.
How to Get It: Food interferes with plasma’s ability to absorb ALA, so it’s best to take a supplement before meals or between meals. Your body naturally produces some––but not enough––and we find ALA in small amounts in foods including spinach, broccoli, tomato, brussels sprouts, organ meats like liver and kidney, and meat. Supplements, however, can contain as much as 600mg.
Manganese
Reduces oxidative stress in mitochondria

Metabolic Role: Manganese is an essential element that reduces oxidative stress in the mitochondria and activates enzymes needed for glucose and fat metabolism. Research on the relationship between manganese and metabolic syndrome is mixed. Still, high levels of oxidative stress are associated with insulin resistance and diabetes, so reducing it may be beneficial in preventing metabolic dysfunction. A study in mice showed that manganese supplementation improved glucose response in diabetes-prone mice fed high-fat diets, likely because of the increased mitochondrial antioxidant activity. Excess free radical production in the mitochondria can generate oxidative stress, and so the ability to scavenge these damaging molecules can improve mitochondrial health and function, leading to more efficient glucose processing.
Manganese deficiency is rare, so it’s unlikely you’ll need to take a supplement. If you get too much regularly, you could do damage over time. Excess manganese accumulates in the liver, pancreas, bone, and kidneys, but the brain is most susceptible to toxicity. Manganese poisoning can cause cirrhosis, Parkinson-like symptoms, and excess red blood cells, which raise the risk of blood clots.
How Much Do You Need: Adult men should get about 2.3 milligrams of manganese daily, and women need about 1.8 milligrams.
How to Get It: One ounce of hazelnuts contains about 1.6 milligrams of manganese. The same amount of pecans is good for 1.1 milligrams. Just three ounces of mussels contains 5.8 milligrams, and brown rice, oysters, chickpeas, spinach, and pineapple also provide about one-third or more of your daily recommended amount of manganese.