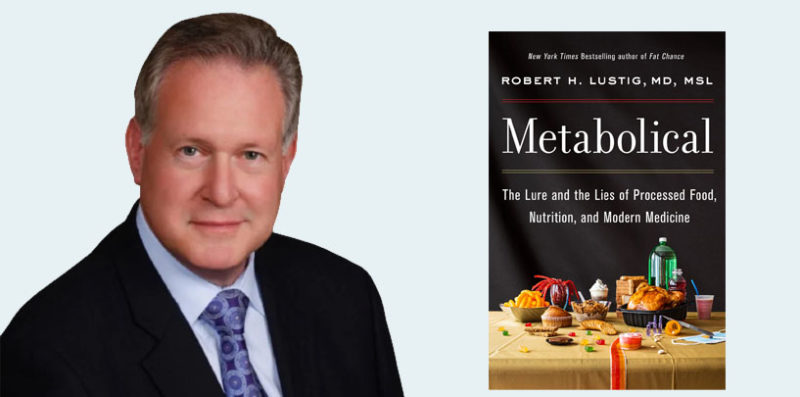
Dr. Robert Lustig is a Levels advisor and the author of six books, including Fat Chance, Hacking of the American Mind, and his most recent, Metabolical. He’s been one of the leading voices in revealing how processed food and sugar are poisoning people and questioning the prevailing views around obesity and metabolic health. He’s a professor emeritus of pediatrics in the division of endocrinology at the University of California, San Francisco, and has authored 135 peer-reviewed articles and 82 reviews.
Dr. Lustig recently joined the Levels community on a video call for the first-ever Levels book club to answer questions inspired by Metabolical. Levels co-founder and chief medical officer Dr. Casey Means began with a few questions and then turned it over to Levels members. The following is an edited version of that session.
On why he’s comfortable being an iconoclast …
Dr. Casey Means: The first question I have for you is how you became the way you are. In your book, you mentioned that exposing the inconsistencies of mainstream medicine and nutritional dogma has made you an iconoclast and has relegated you to the outside of the mainstream medical establishment. But that your commitment to producing high-quality data has kind of been the saving grace to keep your reputation intact.
You’re one of the most independent and critical thinkers in the world today. How did you become this way? And how do you maintain that emotional and personal resilience to continue pushing this ball forward, despite intense pushback?
Dr. Robert Lustig: Look, I’m a doctor, okay. Doctors are supposed to help people. Doctors are supposed to save people. I get a tremendous amount of life satisfaction by seeing a kid do better because of my work and advice.
What I realized growing up is that children are rarely perpetrators, but they are frequently victims. What I saw when the obesity epidemic came around was that children were being portrayed as perpetrators — it was their fault. I knew that wasn’t true. Having been a fat kid myself, I just knew that wasn’t so. So, trying to do right by children has always sort of been my North Star.
In terms of wanting to get it right and making sure that the people who got it wrong got their just desserts, I can think of a very specific episode in my medical school training. I was a third-year medical student at Cornell, and my medicine rotation had two, six-week blocks. We had two different tutors for the six weeks. The first tutor was a famous cancer endocrinologist at Memorial Sloan Kettering. And we would meet with him three times a week, and we all had to present. One week, we had to talk about thyroid function in both cancer and hyper- and hypothyroidism.
Just that week, I had read a new paper on the effects of propylthiouracil, how it blocked peripheral conversion of T4 to T3. And so, I brought that up. And this guy—a cancer endocrinologist and a thyroid oncologist—told me that I was completely wrong, that I didn’t know what I was talking about. So I quoted the paper. And he failed me.
He failed me. The good news was that the second guy gave me honors. So I ended up passing. But I have long had a, shall we say, disdain for authority and recognition that the gurus don’t necessarily know everything.
But to be effective, you have to know what you’re talking about. Everything I do is documented with science; because science is my sword; it’s also my shield. I’ve got a good grasp of the science, and I’m smart enough to make that relevant. So I’ve got a background that tells me: Do right by children and don’t let anybody steer you wrong.
Dr. Means: It’s been disappointing to see that even COVID could not get us as a country to care about metabolic health, at least on a public health level and a policy level. Even though since April of last year, we’ve seen in dozens of research papers that metabolic health is deterministic of COVID outside s.
So, if this couldn’t shift things at the highest levels, what do you think can? And what can we learn maybe from the anti-smoking playbook, which is a bit more of a subtle evolution in changing thinking?
The last part of this question is, do you think that we will get there? Do you think we will become a metabolically healthy country?
Dr. Lustig: Let’s start with the public health challenges in the past and what they mean for our current crisis. Let’s take the most recent debacle: HIV.
HIV set up an enormous conflict between the people who said, “These people were perpetrators,” and the group that said, “These people were victims.” That went on for a long time, for a decade. It wasn’t until we had protease inhibitors, that incidents of HIV started to calm down, and that dialog got forgotten. Now, there’s no issue; it’s gone. This is what happens; this happened during smallpox, it happened with syphilis, it’s happened countless times. When there’s a public health crisis, you get these different factions warring at each other.
This will go away. But the question is, what does it leave in its wake? What it leaves is a medical profession that is damaged. The fact of the matter is we have been damaged for decades. We used to be doctors; now we’re providers. That takes away the respect our patients had for us.
Here’s a way to look at it, and I find this very prescient and disheartening. Max Planck, the famous German physicist, famously said in 1911, “Science advances, one funeral at a time.” He meant that science is held hostage by the gurus at the top, and they have to die before new ideas can come forward.
He said it as an offhand comment, but is it true?
It turns out the National Bureau of Economic Research, headed by Pierre Azoulay at MIT, did an empirical study of that question. They went to the National Academy of Science and the International Institute of Medicine roster for 20 years—from roughly 1995 to 2015—and gathered up all the names of all the gurus and created a database of their papers, as well as their co-authors.
The question was not “What happened to the gurus?” The question was “What happened to the co-authors?” In those 20 years, some of the gurus would have died. So they asked the question, “What happened to the co-authors’ paper productivity after their mentor, their protector, passed away?” It turned out their publishing went into the sewer right after their guru died.
Then the question is, “All right, these people stopped publishing. Well, who was publishing in that field? And what were they saying?” The researchers used MeSH terms on those papers to figure out who is now publishing in that field. It turns out it was an entirely new crop of people with entirely new sets of ideas.
They proved, empirically, science advances, one funeral at a time. I guess I’m an iconoclast because I recognize that some ideas have to be retired or die. There’s a book called This Idea Must Die. It’s got several examples of ideas we thought were absolute dogma and turned out to be completely wrong.
On how we change medical training to address systems-level health …
Dr. Means: Two of the most electrifying chapters of the book, seven and eight, where you talk about the subcellular pathologies that lead to most disease.
This is a systems biology approach, very different from what we’re taught in medical school, which is a labeling approach to medicine. We look at downstream symptoms; we put labels on them; that’s a very convenient way to pick medications or interventions with which we can approach these labels. The systems biology approach helps us realize that diseases are interconnected on the most fundamental cellular level.
So my question is, how do you see the medical system shifting its thinking towards treating the subcellular pathologies that lead to disease and not the downstream symptoms? How is this going to work its way into medical school?
Dr. Lustig: Casey, you have just summed up what’s wrong with modern medicine in a question. I will be frank with you: I don’t have answers to virtually any portions of that question. You’re right, this is a systems biology issue, and we don’t teach systems biology in medical school.
What we teach is how to play Clue. We learned “Colonel Mustard in the Conservatory with the Candlestick.” That’s what we learned. The point is not, “was Colonel Mustard in the Conservatory with the Candlestick?” The question is, “How did Colonel Mustard get into the Mansion in the first place?” You have to find the root causes of problems to solve problems.
The first sentence of the book is, “There’s a wasp in your attic, what are you going to do? Kill the wasp or find the wasp’s nest?” Working downstream of a problem only solves the results of the problem; the problem is still there. That’s what modern medicine does.
How do you get that into medical school? The answer is I don’t have a clue. The reason I don’t have a clue is because pharma controls the medical school curriculum. After all, they underwrite 80% of medical school costs. This will require a groundswell of awakening amongst physicians all over the country—and really, all over the world—to make this happen. There are a whole bunch of obstacles to that occurring. I wrote Metabolical as an impetus, a conversation starter, to get there.
But how to do that? That’s bigger than me. That’s above my pay grade.
On why ultra-processed food is poison and how we get people to recognize that and change behavior …
Dr. Means: There are vast swaths of the country that do not have access to healthy, unprocessed, real food. The system is rigged against them in that unhealthy food is heavily subsidized by the U.S. government, our public food programs promote the eating of processed foods, etc. The system has to change. But there is also an element of personal accountability: when we choose a meal, it has to be this unprocessed real food.
How do you talk about that, and have you landed on an approach that makes the message both practical and compassionate?
Dr. Lustig: I hear you, and I’m not sure I have. I’m not going to tell you that I have been effective. I’ve been effective with a very small percentage of people. I’m not a touchy-feely guy. I’m a give-it-to-you-straight kind of guy.
But I’ve settled on a recent paradigm that seems to be gaining traction. I’ll try it out on you, see how you like it, and see how the audience likes it.
Here we are talking about food. What is “food”? What’s the definition of food? Anybody got a definition?
Audience member: Fuel.
Dr. Lustig: Fuel. Well, not quite, almost, but not really. Try again.
Audience member: Organic matter that can be turned into energy.
Dr. Lustig: Turned into energy. You’re halfway there. If you go to Webster’s and look at the definition of food, it is “Substrate that contributes to either the growth or burning of an organism.” Any substrate that you would use can cause growth, or it can cause burning, but it can’t do both at the same time.
Kind of like a piece of wood in your house: it can be used for building furniture, or it can be used for firewood, but it can’t be used for both. Any specific molecule that you consume can be burned down to carbon dioxide and ATP, or it can be used for its structural components to form lipids, amino acids, ribose, etc., for cell growth. Those are your choices.
There are three enzymes in each cell that determine which way the substrate goes: they’re all kinases, and they have receptors and transcription factors that run them.
So that’s the definition of food. But what if a substrate inhibited burning?
The molecule fructose, the sweet molecule in sugar, inhibits three separate enzymes in mitochondria that prevent burning: AMP kinase, ACADL, CPT1. The primary component of ultra-processed food inhibits burning.
Let’s take growth. If something causes growth, that makes it food. What if the substrate inhibited growth? My colleague, Dr. Efrat Monsonego-Ornan, who is the Chairman of Nutrition at Hebrew University-Jerusalem, just wrote a paper on how ultra-processed food inhibits skeletal growth, calcium accretion and causes inhibition of structural growth. In addition, we know that those same things promote cancer development.
Ultra-processed food inhibits growth and inhibits burning. It’s not food. It’s poison. That’s not taking a disparaging view. That’s taking a very epistemological view of this, and it’s not conferring any sort of social inequity phenomenon. Because lots of elite people eat ultra-processed food, too. But what it’s doing is calling attention to the science and then using the people’s brains to turn that science into rational policy.
On what’s not going to change in the next 10 years …
Lisa: Everybody always asks, “What is going to change in the next 10 years?” My question is, “What’s not going to change and what do we either need to fight or keep up?”
Dr. Lustig:
Thank you for the question. It’s an excellent question. The thing that’s not going to change is social inequality. I think that’s going to inhibit change. The problem is that people use social inequality to raise attention, but they also use it as a bludgeon. That causes problems. It keeps things from moving. This notion, for instance, that taxing soft drinks was regressive against the poor. “A sugar tax or diabetes?” These were the questions coming up as San Francisco, Oakland, and Philadelphia debated a soda tax. The fact of the matter is: no one needs soda, and people would be much better if they didn’t buy any.
And that’s what the tax is supposed to do. It’s supposed to reduce effective availability. The Iron Law of Public Health says reducing the effective availability of a substance reduces consumption, which reduces health harms. It’s true for tobacco; it’s true for alcohol; it’s true for opioids; it’s true for sugar.
So, if you’re trying to get to a reduction in consumption, then reducing effective availability, a tax is low-hanging fruit. But look what came out of that. Chicago passed a soda tax and then repealed it because people cried foul because it was “regressive against the poor.”
We’re going to continue to live with those social inequalities on both sides. And people who can afford better food are already buying better food. We have to make that better food affordable for everyone. And there are all sorts of problems in the current food business model that prevent that from happening. So to fix that, we’re going to have to dismantle the entire food business model. That’s doable, but everyone has to play, and the problem is they don’t want to play. So I don’t think that’s going to get fixed in 10 years.
Gavin: This big community that we have somehow keeps getting crushed by the FDA, Big Food, Big Ag, despite our numbers. How do we unravel these entities that are in such control of these systems?
Dr. Lustig: Well, again, if I knew that, we’d already be doing it. There’s a lot of glad-handing here. Both the FDA and USDA are called what’s called “captured agencies”. The bottom line is that the heads of these agencies come from industry; they go into these jobs and go back to industry. This is the revolving door of influence peddling. Martin Gilens from Princeton wrote this book called Affluence and Influence. Sheldon Wolin, also from Princeton, was one of the biggest proponents of this issue. He wrote a book called Democracy Inc, arguing that the corporate entities and the government become the same entity. If you look at the Trump administration, that’s exactly what happened. So we have to dissociate those.
But I’m not that politically savvy to know how to fix that. This is one of those things where you can identify the problem, but identifying the solution is much, much more problematic. We don’t have the rules in place to vet people before they go into these positions. It’s all politically gamed to start with. So, the best I’ve got is science.
One of the lynchpins of this is this concept called the calorie. If it’s about calories, then it’s about what’s in the food. And what’s in the food can be done by the head of the USDA. We have to change that model. The point of the book is that the food processing is more important than the actual ingredients. And, nobody who runs the USDA knows anything about that. We have to get some people who do know something about that in there. How’s that going to happen? Who’s going to appoint them? I don’t know how to do that. I’d like President Biden to rethink that. He reappointed Tom Vilsack as head of USDA. That was a disaster the first time, and it’s a disaster again.
You’re asking the hardest question. And I just don’t have an answer.
On the price society pays for processed food …
Christina: How is bad food the cause of societal devolution?
Dr. Lustig: Bad food is a cause of societal devolution in two ways: demographics and biology. Let’s start with biology first. There are two chemicals in your brain that help grow neurons: leptin and brain-derived neurotrophic factor, BDNF. You are smart because both of those work. But what if they didn’t work?
Well, guess what stops them from working? Insulin and fructose. Bad food, as the generator of hyperinsulinemia and the source of added sugar, inhibits the trophic actions of these chemicals on your neurons. That leads to individual devolution, which then leads to societal devolution.
The second reason is more at a societal level. I asked the director-general of the WHO, Jose Gonzales De Silva, the following question, “Which is worse, no food or bad food?”
Anybody want to venture a response to that, which is worse, no food or bad food?
Audience member: I’m assuming he said no food.
Dr. Lustig: He didn’t say. He didn’t have an answer. Or maybe he just was adept at sidestepping the question.
“No food” starts wars, right? And wars kill people, but they kill a certain number. And then the war ends. And then, presumably, some new social structure comes along, and now there is food. So there’s no question that “no food” is bad. Of course, it’s bad.
But what about bad food? Bad food chews away at the edges for so long. It’s like the frog in the boiling pot: you don’t even know what’s happening.
It ends up doing just what happens in frog boil. It creates a torpor of society so that it doesn’t even know what’s going on. Anybody see the movie, Idiocracy? Terrible movie, horrible movie. Good premise, horrible movie. Guy wakes up 200 years later, finds out he’s the smartest person on the planet. Everyone is drinking Kool-Aid out of the faucets. But that’s what’s happening; it’s actually happening. That’s how social devolution also occurs.
On identifying the worst processed food …
Scott: Not all packaged goods seem to be created equal. Think of frozen raw salmon versus frozen DiGiorno pizza. Is there some sort of truth on how processed various foods are? If we’re trying to protect the liver and feed the gut and need some convenience foods, who do we turn to?
Dr. Lustig: Great question. Very practical. There are a couple of things. The book makes it very clear: It’s not what’s in the food; it’s what’s been done to the food. And that’s not on the label. I think that’s what should be on the label because all food is inherently good. It’s what we do to the food that’s not. By inhibiting growth or burning, as we talked about, that’s what turns food into poison. Those things have been done to the food because it was food until the food industry got done with it. So how are you going to learn that?
There are a few clues. I am delighted that they have added a line to the nutrition facts label. Under “Total sugars,” it now says “Added sugars.” The Trump administration deep-sixed that for five years. It was supposed to happen in 2016 under Obama. Trump deep-sixed it, but some companies did it voluntarily. By next year, all foods should have that added sugars line. That’s one of the keys because that tells you what they did to the food. The higher that number, the worse it is.
The second one requires a little bit of math. Look at total carbohydrates, and then you look at the dietary fiber. Because stripping away fiber is one of the ways that you starve the gut. Now you’ve got inflammation, now you’ve got leaky gut, now you’ve got all of these other processes that ultimately lead to systemic insulin resistance and, therefore, chronic metabolic disease. What you’re looking for is a total carbohydrate-to-fiber ratio of less than five to one.
That will tell you how much of the fiber that carbohydrate came with got stripped away by the food industry. So that’s a good way of assessing what’s been done to the food also.
Then, of course, you look at the ingredients list, and if sugar is one of the first three ingredients, it’s a dessert. And as the number of ingredients goes up, the risk of ultra-processing goes way up. Any packaged food that you buy that has more than three ingredients has been ultra-processed.
Scott: We’ve had a lot of discussions internally about providing something like a “Levels Approved” stamp, just like there’s like a Whole 30 stamp.
Dr. Lustig: We’re working on that through my nonprofit, Eat Real. We’re going to call it the Metabolical Stamp.
Another thing like that: I am the Chief Medical Officer of a company called Perfact. It’s a digital database of everything on the food label in every store, in every country in the world. You can use it to scan an SKU and know, while you’re in the store, whether or not that food will interfere with your biochemical profile.
For instance, let’s say you have metabolic syndrome and gout, and kidney stones. If you go into the store to buy something, how will you know what to buy? You have no clue. Perfact will say, “You need a low refined carbohydrate, low sugar, low purine, low oxalate diet.” Let’s say you want chicken cacciatore for dinner. You type that in, and it matches your biochemical profile, then accesses a database of a million recipes and finds the 20 chicken cacciatore recipes. It then figures out which ones are the lowest in refined carbohydrate and sugar, which is the lowest in purine, and which is the lowest in oxalate. Then it goes to your supermarket, looks for the ingredients that meet your biochemical criteria, orders those, delivers them to your house, and charges your insurance company for the cost of the food. Because if you eat that, then you won’t need the allopurinol, you won’t need the lithotripsy, and you won’t need the oral hypoglycemics.
That’s personalized nutrition. Monitoring glucose is the first step in personalized nutrition. That’s why I’m happy to be an advisor for Levels. But that’s the first step on a thousand-mile journey.
On teaching kids how to choose good food …
Scott: My three-year-old is on her second day of pre-school today. And we’re trying to sort out what food we send her. At Levels, we’ve got a lot of work to do with adults, who have all the agency we could ask for. But as you start going down the age range, it becomes a whole different level of responsibility for parents to feed their kids.
Dr. Lustig: Absolutely. That’s another reason why kids have to become agents for themselves. I was approached just this past week by two separate entities—the University of Alabama, Birmingham, and a public health collaboration in the UK—to develop a K–12 curriculum with metabolic health as the North Star. How to use it to educate kids who can become the positive, disruptive force in the house.
Which is what we did with bicycle helmets and seatbelts and drunk driving. Thirty years ago, if a politician had stood up in a statehouse or Congress or Parliament and proposed anything against those three things, they’d have been laughed right out of town. “Nanny state, get out of my kitchen, get out of my bathroom, get out of my car!”
Today they’re all facts of life. If you pull out of your driveway and haven’t put on your seatbelt, your kids will scream at you. Did I yell at my parents for not wearing the seatbelt? I didn’t know what a freaking seatbelt was!
That’s how you affect change. You teach the kids, the kids grow up, they vote, and the naysayers are dead.
On why food affects COVID outcomes and blaming people for obesity …
Natalie: So the SweetGreen CEO Jonathan Neman came out publicly and had some thoughts on the pandemic, connecting it to unhealthy eating and junk food. And he got some criticism for that. I was curious about your reaction to that.
Dr. Lustig: First of all, he’s not the first person to say it. I said it, too. I said it last year as part of my nonprofit Eat Real’s medical alert on metabolic health and COVID. We took the CDC and the NIH to task because they told us there were three things we could do to prevent COVID: Masking, social distancing, hand-washing. And those things are still there, right? There’s one they missed, and it was real food.
How does real food make a difference? Real food won’t stop you from getting infected, but it will prevent you from dying. There are three things that processed food does to make COVID infectivity and virulence worse. One, insulin increases the portal that the virus uses to infect you. It’s an endocrine receptor called ACE2. Insulin increases the number of ACE2 molecules on any cell in your body because ACE2 has to do with water transport. High insulin causes water retention. High insulin—due to metabolic disease and ultra-processed food consumption—increases how fast COVID will spread throughout your body because you’ve given it more portals to do so.
Number two, high blood glucose: hyperglycemia, fructose consumption, insulin resistance, metabolic disease. It turns out glucose crystallizes around the edges of that ACE2 and holds it open so it can’t close. It gives the virus an easier path to inject its RNA.
Finally, number three, short-chain fatty acids. Fiber becomes short-chain fatty acids in the intestine, which are both anti-insulin and anti-inflammatory. They suppress the cytokine response, so it doesn’t go hog-wild. We’ve learned that the cytokine response is what kills you during COVID. It’s not the virus. It’s the cytokine response. That’s why steroids, dexamethasone, has been effective in treating severe COVID in the ICU.
Suppressing your cytokine responses is essential. You need short-chain fatty acids, which means you need fiber. Well, guess what’s been taken out of the processed food? Fiber. Ultra-processed food is the single worst thing you can eat during a pandemic like this. And of course, that’s what everyone’s eating. That’s what’s missing from the store. Kraft can’t keep up with the macaroni and cheese, all right? But is the NIH and the CDC talking about it?
I said this before Neman did. The difference is, I didn’t blame the obese person. If you read what Neman said: “78% of hospitalizations due to COVID are obese and overweight people. Is there an underlying problem that perhaps we have not given enough attention to?”
Now, that’s true. But by saying it the way he said it, he made it clear that it’s the obese and overweight person’s fault. And that’s how he got in trouble. Not because what he said was wrong, but because he blamed the victim. And that’s what everyone does. They blame the victim. I don’t. And if Neman had not blamed the victim, maybe he would have gotten a real conversation started instead of getting his head handed to them.
On the best and healthiest steak …
Natalie: One more question: What’s your favorite cut of steak?
Dr. Lustig: I love filet mignon. I put it in a cast-iron skillet with some butter and some mushrooms and carrots and pearl onions. I sear it first and then put it in the oven at 325 for 35 minutes. And it is phenomenal. The other thing I do on the grill is skirt steak with a dry rub. And with broccoli or braised fennel.
Grass-fed tastes as good as corn-fed, but it’s a little tougher because there’s not that much fat. The cattlemen prize their corn-fed beef for being able to be cut with a butter knife. That’s a problem. That means you’ve got so little intramyocellular lipid that it’s not holding together. The fibrous tissue is not holding the steak together.
Those animals are sick. A picture in the book shows Italian beef, Argentinian beef, and US corn-fed beef. You can see the difference in terms of the marbling. But in fact, the Argentinian and Italian steaks are delicious. Argentina and New Zealand eat double the amount of beef we do. We eat 23 kilos a year. They eat 44 kilos a year. And they have a lower incidence of heart disease and diabetes than we do. Ain’t the beef.
On the benefits and limitations of CGM …
Tina: Have you worn a CGM?
Dr. Lustig: No. I haven’t. I’m working my way up to it. I am very clear that the mean glucose excursion published for any given food is the mean, not the 95% confidence interval. There are a lot of people on either side of that. And it does matter because the glucose excursion is related to the insulin response. I’m all about getting that insulin response down, no matter what. So I understand that.
Having said that, glucose is just the start. It’s what we can measure now. I’m glad Levels is doing it. But it is just the start.
There are a lot of other analytes that are going to end up being important. In fact, I think glucose is only about 10% of the story. Insulin will be about 40% of the story. Postprandial triglycerides will be in enormous part because that’s telling you what your intestine is doing with the food.
Lastly, I think lactate will be a big part of it as well. So the question is bringing those channels for those analytes on board. If glucose is only 10%, maybe we need insulin first. I’m working with some other people to bring that to fruition. I had a meeting with one of them just this week, and he thinks we’re five years from market.
On home cholesterol tests …
Tina: You mentioned postprandial triglycerides. There are lots of home tests that you can do. Would you recommend doing a blood sample a couple of hours after you eat?
Dr. Lustig: No, because those tests right now don’t distinguish between chylomicrons and VLDL. Chylomicrons are what happens to dietary fat. They’re huge. They go to the liver and get metabolized. If you’re just drawing a blood sample, you don’t know if it’s the chylomicrons or the VLDL. VLDL is what the intestine does to sugar to get it out. So it absorbs some fructose, and it goes straight via the portal vein to the liver. A recent paper in Nature showed that fructose increases the number of links of the villi in the intestine to increase absorption.
VLDL coming out of the intestine will be valuable, but distinguishing that from chylomicrons will be important. So doing it with the home test isn’t going to tell you anything yet.
On what he’d do if he were in charge of public health …
Tracey: If you were in charge of public health, what would your guidelines be to be American people?
Dr. Lustig: If I had Aladdin’s genie and I had two wishes? One wish for the populace, one wish for the government.
For the populace, the question is, what would you tell them to make them change their behavior? People out there think it’s about obesity. And because they think it’s about obesity, they think it’s the patient’s fault.
What I would say to them is, 20% of obese people are metabolically healthy. They will live a completely normal life, die at a completely normal age, not cost the taxpayer a dime. They even have normal length telomeres, the edges of the chromosomes that determine life span.
Conversely, 40% of the normal weight population have the same diseases as do the obese. Normal weight people get Type 2 diabetes, hypertension, lipid problems, cardiovascular disease, cancer, dementia, polycystic ovarian disease, fatty liver disease. They get it at a lower frequency, 40% versus 80%. That’s true. Obesity is a risk factor. I don’t argue that. But if 40% of the normal weight population have the same diseases for the same reasons, how can it be about behavior?
This looks more like exposure. This looks more like cholera or influenza, tuberculosis or COVID-19 for that matter. When you do the math, it turns out they’re more thin-sick people than there are fat-sick people. If you stop calling the fat-sick person the problem, well, then where’s the problem. Maybe it’s you.
This concept of metabolic health can then expand because people get off this notion that it’s about obesity. Taking obesity off the table as a public health issue and never mentioning the word obesity again would be where I would start.
From a population, public health standpoint, obesity is a red herring. It’s taken us down the wrong road. Metabolic health is the issue. And 88% of Americans are metabolically ill. That’s the public health message I would give.
What would I do if I had a magic wand that could do something with the government? One thing: get rid of all food subsidies because they distort the market.
If you subsidize one thing, you have to tax everything else. That distorts the market. It’s one of the reasons processed food is cheap, and real food is expensive. The consumer price index demonstrates very clearly this is because of food subsidies. Of course, that’s what the processed food industry uses because it’s the cheapest available. Then, of course, sugar is addictive, so that ratchets up their profits like crazy.
But if you took the sugar subsidy away, it wouldn’t be as cheap for them to do it. And therefore wouldn’t be as profitable for them to do it. What would happen to the price of food if we got rid of all food subsidies?
Well, the Giannini Foundation at UC Berkeley did this exercise several years ago. They found that only two things in the grocery store would go up; everything else would stay the same. Those two are corn and sugar—the stuff we want to go up because we’re trying to reduce effective availability. So that’s what I would do for the government: Make the argument for eliminating all food subsidies. But of course, the food industry does not want that.
On why it’s ultimately all about insulin …
Tracey: Is there something that people are converging on around metabolic health? Is there a way that we could shift from obesity to a different, obvious metric?
Dr. Lustig: Fasting insulin. That’s how you know.
Now the problem is that the ADA, the American Diabetes Association, tells you don’t draw fasting insulin. They’re on record for decades now saying, don’t draw fasting insulin. Why am I telling you fasting insulin is the most critical test of all, and they’re saying don’t draw it?
Why do they say what they say? Two reasons, and both of them are wrong. The first is they’ll say, “Well, fasting insulin levels assays across platforms and companies are not standardized.”
That’s true. Some people do it with HPLC. Some people do with radioimmunoassay, et cetera, et cetera. And the antibodies for most of these are not discriminatory. So they pick up other things. The main thing they pick up is proinsulin. Proinsulin is the precursor of insulin. When your beta cell is ultimately stressed, it has to put everything out it can. You have to cleave the C-peptide out of the proinsulin to get the insulin. The beta-cell doesn’t have time because you’re glucotoxic because you’re hyperglycemic. So it’s putting out proinsulin, and that gets picked up in the insulin assay. That’s true.
Who cares? So what? It’s high. That’s all you need to know. It’s high. So what that it’s not standardized?
Reason number two: They say, “fasting insulin levels don’t correlate with obesity.” That’s right. They don’t. They correlate with metabolic health. That’s what they correlate with. They correlate with the risk for diabetes. And as I just told you, 40% of the normal weight population are metabolically ill in the same way that the obese are. But they’re not obese because the amount of subcutaneous fat you carry is irrelevant to your metabolic health. It’s the amount of ectopic fat you carry in your muscles and in your liver that matters, and you don’t measure that on the scale. So the fact that fasting insulin does not correlate with obesity is precisely why you have to measure it.
The American Diabetes Association is wrong on both counts. And I’m doing my absolute utmost to call them out. But do you think they’ll ever have a debate with me?
On the challenge of turning individual data into science …
Dr. Lustig: Let me give you one last thing. Levels is 80,000 Ns of one. Ns of one are not science. But there are ways to turn those 80,000 Ns of one into science. And that’s Levels’ challenge. It’s why I’m here to help. This is a wonderful way to capture this information. Now we have to use it to generate science, to fix the problem across the board. We can do better. And we will.